Although more children than at any point in history are now protected against vaccine-preventable diseases, millions of zero-dose children are still missing out on the life-saving benefits of immunization entirely. These children often live in the world’s most marginalized communities where inequities are clustered and compounded by poverty, geography, gender, and conflict. In order to keep making progress against preventable deaths and illness, leaders will need to integrate equity across global, national, and sub-national immunization strategies.
Key Messages
- Health inequities are “the unjust differences in health between persons of different social groups, and can be linked to forms of disadvantage such as poverty, discrimination and lack of access to services or goods,” as defined in the WHO Handbook on Health Inequality Monitoring.
- Both between and within countries, vaccine coverage is often distributed unequally across populations – those in the highest socioeconomic status groups and those with the most education often have the highest immunization rates while marginalized populations, those living in poverty, and those with lower education have the least access to immunization.
- Improving equitable access to vaccines aligns with achieving the Sustainable Development Goals.
- Prioritizing equity requires multisectoral strategies designed to reach communities that have previously been excluded from access to health services based on geography, educational status, and sociocultural group.
Compounded Vulnerability
Record numbers of children are protected from preventable illnesses thanks to immunization, yet millions of children, often the poorest and most vulnerable, continue to be left behind. Vaccine-preventable diseases disproportionately affect those who experience both poor overall health and low economic standing; the children who miss out on life-saving vaccines are often those in the poorest households and the most remote locations, and whose families lack access to clean water, education, and adequate nutrition.
Over 13 million ‘zero-dose’ children have never received any vaccines at all, based on a 2019 analysis from UNICEF. These children and their families already experience a disproportionate burden of vaccine-preventable illnesses like measles, diphtheria, and polio. With life-saving immunization services around the world disrupted by the COVID-19 pandemic, these children are at even great risk from disastrous outbreaks of vaccine-preventable illnesses.
On June 4th, 2020 the Global Vaccine Summit will aim to raise at least $7.4 billion for Gavi, the Vaccine Alliance. This funding will help support the mass vaccination campaigns and rebuilding of health systems needed over the coming years to help address the damage done by the COVID-19 pandemic. Gavi’s strategic plan for 2021-2025 prioritizes immunization equity and the need to reach the communities that have missed out on previous immunization efforts, especially those most marginalized by poverty, geography, and conflict.
Combating inequities in health and wealth through immunization
Evidence has shown that vaccines have the greatest health and economic benefit amongst the poor. Globally, the poorest populations often experience the worst impacts of vaccine-preventable diseases, both in terms of health burdens in illness and death as well as carrying potentially crushing costs associated with medical care, missed work, and lasting disability.
Research shows that vaccines are one tool that can help break the pernicious cycle of poverty and ill health, improving equity across both health and wealth. By preventing disease, vaccination also prevents the costs associated with medical treatment and thus helps to reduce the likelihood that households will fall into or remain in poverty.
- A 2018 modeling study of the economic impact of 10 childhood immunizations in 41 low- and middle-income countries found that with the lowest income households received the greatest financial risk protection from costs of measles, pneumococcal disease, and rotavirus. The authors conclude that: “Including equity components into economic evaluations will allow policy makers to opt for interventions that target specifically the most vulnerable populations.”
- A 2015 study from Ethiopia looking at the impact of pneumococcal vaccine introduction in Ethiopia found that 30-40% of all deaths averted would be expected to occur in the poorest wealth quintile. The greatest resulting financial risk protection would also be concentrated among the lowest income quintile.
- A 2018 cost-effectiveness analysis found that expanding rotavirus vaccination coverage among the poorest and most vulnerable populations of children would substantially increase the overall impact of rotavirus immunization in Pakistan; children in the poorest households would experience a three to four times greater mortality reduction benefit compared to children in the richest households.
Empowering and educating women can lead to greater rates of vaccination among children
Although girls and boys are immunized at similar rates globally, barriers that inhibit women’s ability to access healthcare and immunizations for their children may still exist at subnational levels and across different populations. Research in several LMIC contexts has found that access to education, particularly for women and girls, is often strongly associated with higher rates of immunization in children.
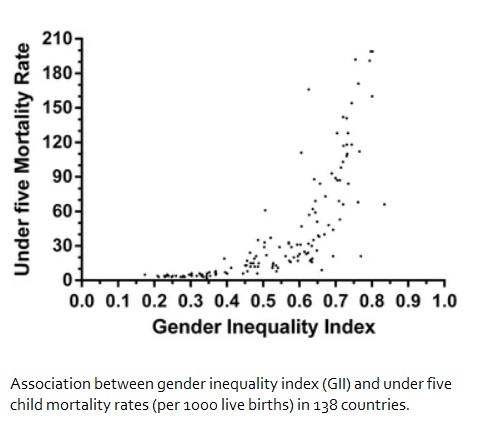
- A 2015 ecological study of 138 countries found that greater gender inequality was significantly correlated with lower immunization coverage and higher neonatal, infant, and under-5 mortality.
- A 2018 study in Nigeria found a robust association with maternal education and immunization coverage for children at both the individual and at the community levels. The researchers concluded that maternal education had a spillover effect that benefited immunization rates of all community members, not only a mother’s own children. This suggests that even children of uneducated mothers can benefit from the education of women in the community overall.
- A 2017 systematic analysis of equity in vaccine coverage across 45 low- and middle-income countries found that maternal education is a strong predictor of child vaccine coverage. Children of the least educated mothers were 55% less likely to have received measles vaccine and three doses of DTP vaccine compared to children of the most educated mothers.
- A 2015 review of health equity and disparities data from Demographic and Health Surveys and Multiple Indicator Cluster Surveys conducted in 70 developing countries found that “with respect to immunization, the greatest disparity exists for children born to women with no education compared with those born to women with secondary (or higher) education.” The global coverage of the third dose of DTP is 26% higher among children born to mothers with some secondary education compared to mothers with no education.
Geography and Sociocultural inequities and the immunization gap
Where a child is born often dictates their access to health resources like vaccines. Despite improvements in vaccination rates at the national level, local level disparities continue to persist. This means that children born in remote, rural, or urban slum settings may have significantly less access to immunization compared to their peers born in urbanized settings near health facilities. Inequities also exist for marginalized populations and minority groups who may have restricted access to health services such as immunizations. Conflict and migration are additional factors that threaten access to immunization for many children and their families.
These inequities in vaccination rates—often concealed in national averages—call for special efforts to improve immunization rates in this rapidly growing sub-population to reduce both health inequities and the risk of infectious disease outbreaks in the wider society.
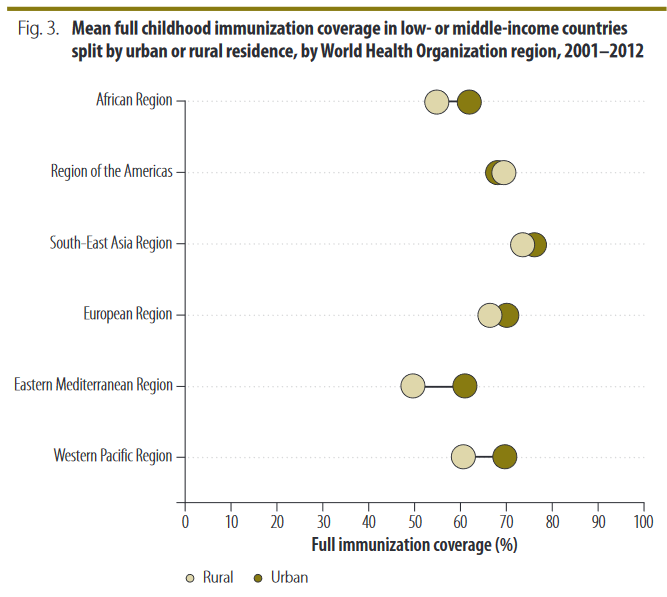
- A 2015 immunization equity review found that globally, coverage of the third dose of DTP among 1-year-olds is 8% higher among urban dwellers compared to children living in rural environments.
- Children from families that have migrated from other parts of the country have less access to health services and lower vaccination rates compared to the general population. According to a 2016 systematic review and meta-analysis, children who are rural-urban migrants in China, India, and Nigeria were less likely to be fully immunized by the age of one year than non-migrant urban residents and the general population.
- A 2019 study in New Zealand found that the use of pneumonia conjugate vaccines (PCV) appears associated with reductions in ethnic and socioeconomic disparities in invasive pneumococcal disease (IPD), all-cause pneumonia (ACP), and otitis media hospitalization among Māori and Pacific children. Following the introduction of conjugate vaccines in the country, Maori and Pacific children’s rates of admission for IPD dropped by 79% and 67%, respectively.
- A 2019 study examining immunization rates in urban and rural populations in Tanzania found that wealth and mother’s education were significant predictors of vaccination rates in both urban and rural settings. However, low paternal education, lack of antenatal care, and home births were significantly associated with low vaccination rates only in rural settings, suggesting a need for tailored vaccine programs.
- The results of a 2016 cross-sectional polio serosurvey found that the Jordan Ministry of Health’s proactive campaign to locate and vaccinate high-risk populations has been successful in maintaining high population immunity—even with a recent influx of refugees from Syria. The study included a community sample of 479 children under 5 years old living in areas of Jordan identified as high risk due to being hard-to-reach, having high numbers of refugees, and lower vaccine coverage (under 90%).