Undernutrition and infectious diseases are tightly linked in a self-reinforcing cycle. Childhood episodes of diarrhea, pneumonia and measles are exacerbated by undernutrition, which significantly contributes to the death toll from these infections. In this feature, the VoICE team explains the cycle of malnutrition and infectious disease, and brings you evidence of the ways in which vaccines interrupt this cycle and help to protect the overall health, growth and physical development of vulnerable children.
A selection of VoICE evidence in this issue
A hidden killer: poor nutrition underlies almost half of all deaths in children under 5
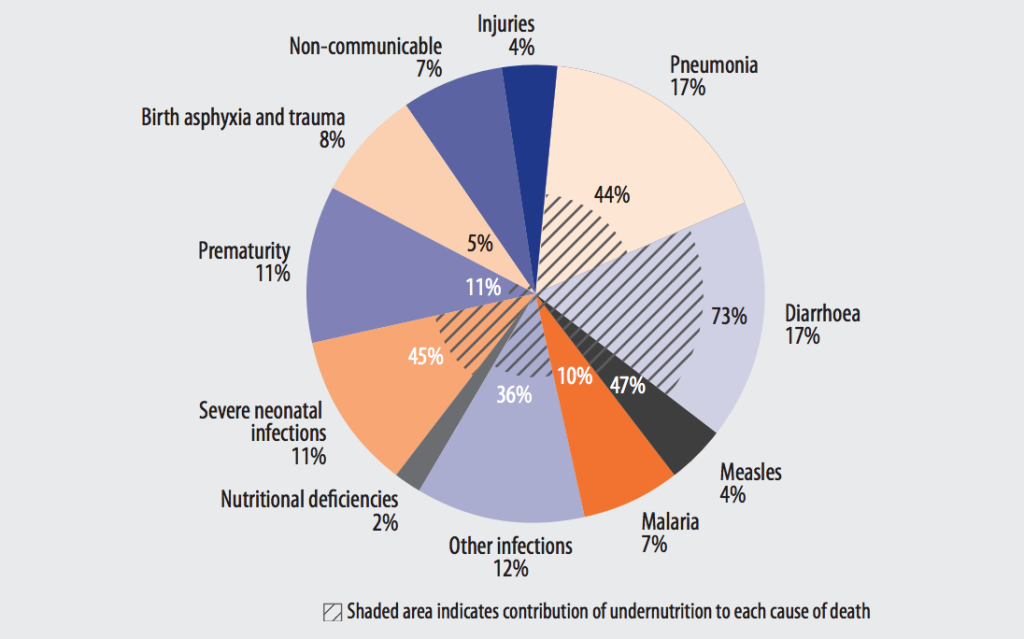
You won’t see nutrition listed as the cause of death in a pie chart of child mortality, but undernutrition is one of the key contributing factors behind child deaths due to infection. Undernutrition is defined as insufficient food intake—including calories and/or nutrients–to sustain growth and health. (Malnutrition, in contrast, is a broader term referring to both undernutrition and overnutrition—the excess intake of food and calories.) The WHO estimates that undernutrition is a factor in 45% of child deaths—contributing to over 3 million deaths in 2004 – including 73% of child deaths due to diarrhea, 44% of pneumonia deaths, 47% of measles deaths, and 45% of deaths due to severe neonatal infections (Figure 1).1, 2, 3 These are the top childhood killers, and they share a recurring theme: undernourished children get sick more often and have worse outcomes—including a higher risk of dying—from every episode of infectious disease.4
Figure 1: Major causes of death in children under 5 years old with disease-specific contribution of undernutrition, 20041
Many children worldwide are still undernourished
Undernutrition is common among children under 5, particularly in the poorest regions of the world, such as South Asia and Sub-Saharan Africa where 1 in every 3 children is undernourished. 5Undernutrition manifests in different ways as stunting, wasting and specific nutritional deficiencies of key vitamins and minerals that children need to grow and develop properly.
Stunting, as defined by a recent report from the WHO, UNICEF and the World Bank, refers to a child who is too short for their age.5 It is a result of chronic or recurrent undernutrition and affects 23% of children globally, or 155 million. Three-quarters of stunted children live in Sub-Saharan Africa and South Asia, where the prevalence of childhood stunting exceeds 33%. A more acute form of undernutrition is wasting, which refers to a child who is too thin for their height. Wasting results from rapid weight loss or a failure to gain weight and affects about 8% of children, or 52 million, under 5 globally. However, in South Asia levels are particularly critical with over 15% of children under 5 experiencing wasting.5 Notably, stunting is more prevalent than wasting as it is cumulative after multiple, shorter episodes of wasting—which in and of themselves can be reversible—but over time leads to stunting which is largely irreversible and has lifelong consequences.6
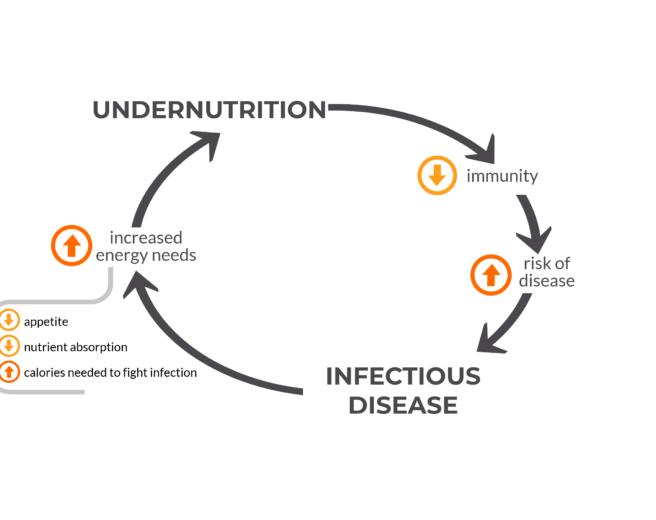
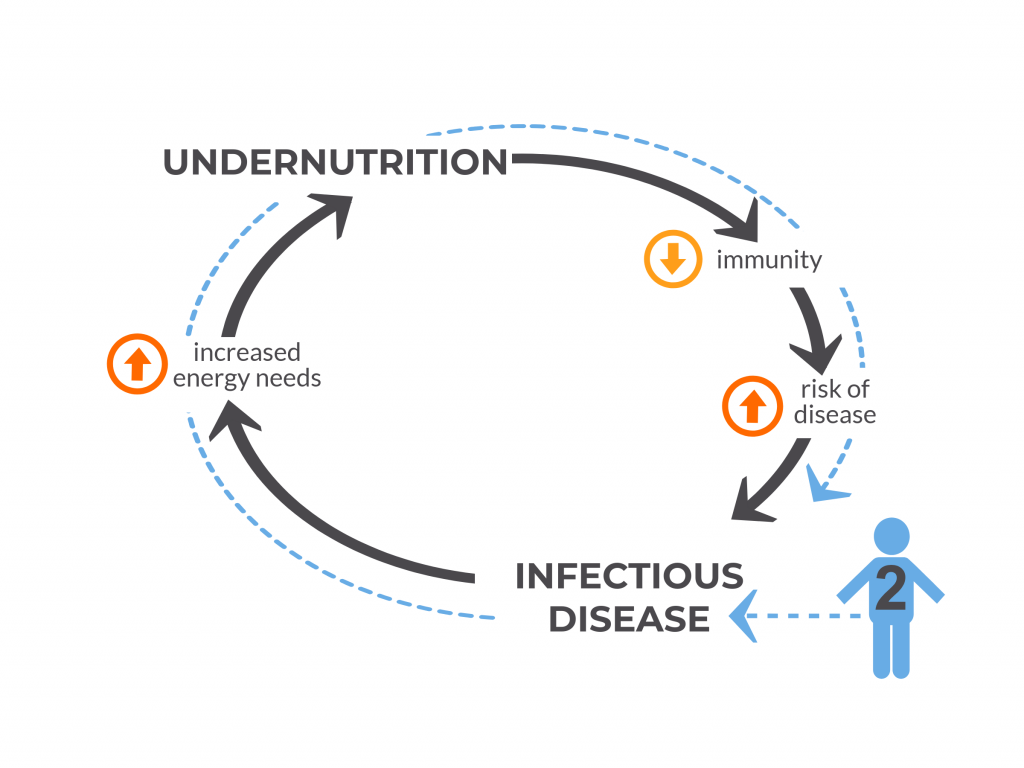
A vicious cycle: undernutrition and infection
Figure 2: The vicious cycle of undernutrition and infectious disease
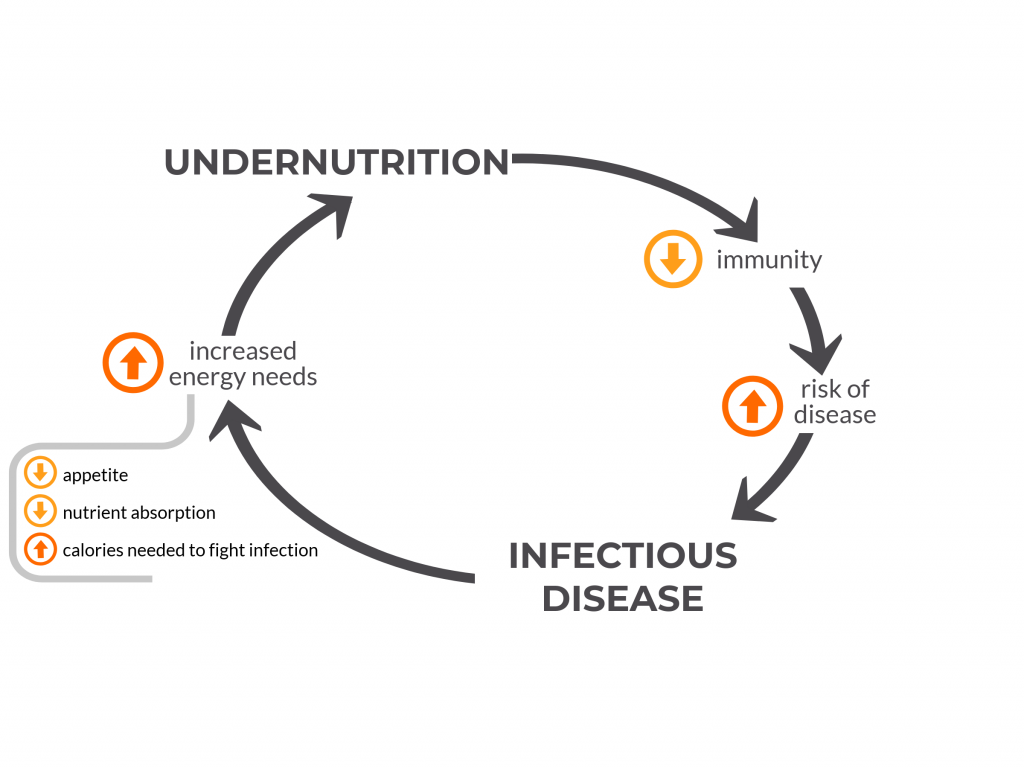
Undernutrition has been called the most common cause of immunodeficiency worldwide.7 With poor nutrition, some parts of a child’s immune system do not function properly. The skin and gut cannot effectively block disease-causing bacteria, viruses and parasites from entering the body. The thymus, a gland in the neck which helps develop the disease-fighting T cells, becomes smaller and other parts of the immune system do not function properly. Thereby undernourished children are put at increased risk of developing diseases to which they are exposed in their environment and against which they otherwise would normally be able to defend themselves.
With each episode of disease, some of the energy and calories a child would otherwise use for growth and development is diverted to fight off the infection. Calories are consumed to mount a fever, one of the body’s protective mechanisms. If the child has pneumonia, breathing requires more work and this will require more calories, too. If the child has diarrhea, less nutrients are absorbed while the gut is inflamed and infected. For these reasons, a sick child needs more energy and calories to fight off the infection and recover, and an undernourished child – who has fewer energy reserves and likely less access to nutrient-rich food to begin with – falls even further behind in fulfilling their nutritional needs and is more susceptible to the next bout of illness.8
Figure 3: Child #1 is Undernourished
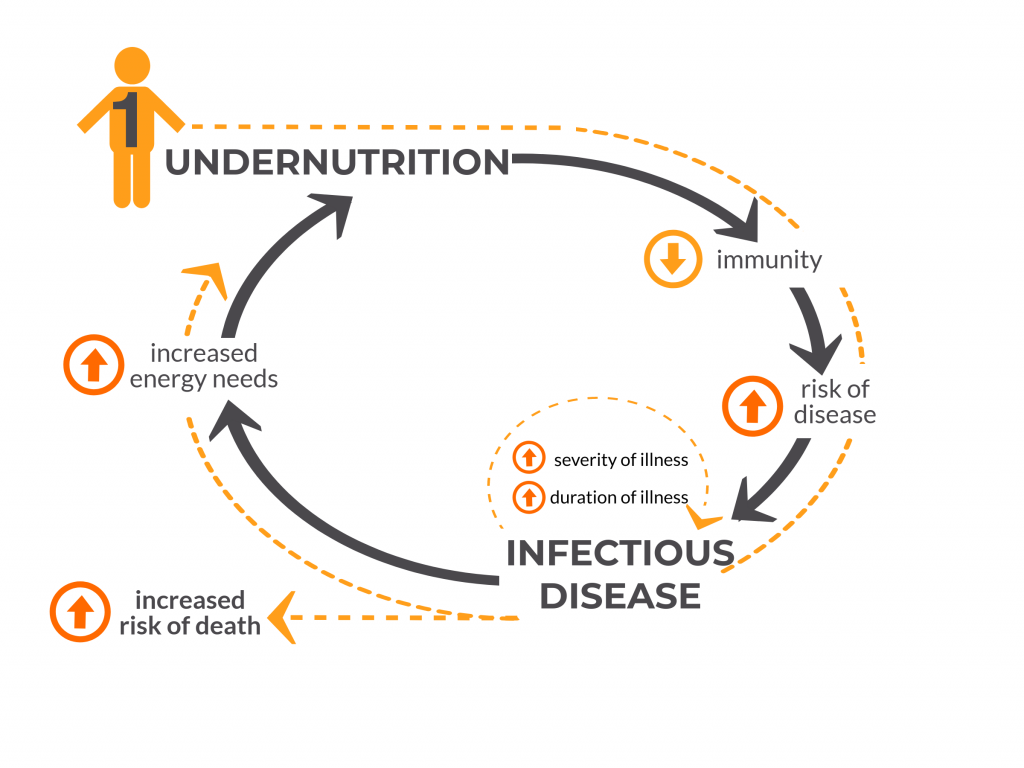
A child who is sick also may not eat as much, taking in fewer calories and nutrients for the duration of the illness, putting the child at risk for falling further behind in growth. A prospective case-control study conducted in several developing countries found that children with moderate-to-severe diarrhea grew significantly less in length in the two months following their episode compared to age- and gender-matched controls.
Not only are undernourished children – like child #1 in Figure 3, above – more susceptible to getting sick, but their disease course is more likely to be severe or even fatal. A study of Bangladeshi children found that severely undernourished children had a nearly eight-fold increased risk of death from diarrhea than those who were not severely undernourished. In the case of pneumonia, those who are undernourished are at a 15-times higher risk of death. In this way, undernutrition is a hidden co-killer, masked behind the number of deaths due to diarrhea, pneumonia and other infections such as measles and malaria.
An otherwise healthy child – like child #2 in Figure 4, below – can also become temporarily undernourished because of an infection such as pneumonia, due to the increased energy needs of the infection. This can put the child at increased risk of other infections until a healthy nutritional status is attained once again.
Figure 4: Child #2 was not undernourished, but became undernourished due to an episode of infection.
Sickness and undernutrition have long-term consequences for children’s growth and development
Recurrent disease, severe disease and undernutrition interact to shape the trajectory of a child’s growth and cognitive development in the critical first 1000 days of life with long-term implications. Certain severe infections such as meningitis leave many children with long-term cognitive impairment and neurological sequelae. In a systematic literature review of studies from Africa, it was found that one quarter of children who survived pneumococcal or Hib meningitis—two vaccine-preventable causes of meningitis–had long-term neuropsychological deficits.
Stunting has been linked with lifelong consequences such as diminished cognitive development and decreased economic productivity for affected individuals.8 Studies have estimated that undernutrition decreases a nation’s economic growth by 8% or more due to the reduced potential of its people to study or work to their full potential.9
Vaccines are an important component of breaking the vicious cycle
The interactions of childhood diarrhea, pneumonia and malnutrition contribute to a vicious cycle of poor health and delayed growth and development. Immunization, as an effective measure to protect against some of the main diseases of childhood, can help to disrupt this cycle.
Vaccines for pregnant women
The pathway to undernutrition often begins early, even as early as pregnancy. In this period of fetal growth and development, a mother’s receipt of influenza vaccine has been associated with improved pregnancy outcomes. In a US study, there was found to be an association between immunization with the inactivated influenza vaccine during pregnancy and reduced likelihood of prematurity and small for gestational age birth during influenza season. Another review demonstrated that influenza vaccine during pregnancy adds 200 grams to newborn weight and reduces low birth weight by 15%. Reducing prematurity and improving fetal growth translates to a reduced risk of stunting in young children.10
Infant vaccines
Pediatric vaccines recommended by the WHO and UNICEF have been proven safe and effective in reducing children’s risk of disease and death. Vaccines such as pneumococcal conjugate vaccine (PCV) and Hib conjugate vaccine target bacteria that cause pneumonia and meningitis. Live, attenuated rotavirus vaccines target the leading cause of severe, dehydrating diarrhea in young children.11
Even children who are undernourished can respond well to vaccines, though there may be some differences in the amount or type of immunity they can produce depending on the degree of their undernutrition.9 More up-to-date studies are needed on the immune effects of undernutrition as much of the data on this topic is from older studies and using older laboratory tests. However, vaccines given to children on a timely basis have significant benefits for malnourished children and are integral in a multifaceted approach to breaking the vicious cycle of undernutrition and disease. In addition, many vaccines trials have been conducted in populations with high rates of stunting and wasting and have proven that even in these settings vaccines are effective and highly impactful.12, 13, 14, 15
By reducing the frequency of disease in at-risk children, vaccines help undernourished children maintain their nutritional status and use their calories for growth and cognitive development. In a review of recent studies, researchers show that PCV7 given to infants translates into an additional 500 grams of growth in the first 6 months of life. Another study in Kenya found immunization with polio, DPT and measles reduced the proportion of children under 2 years of age with stunting by 27%.
Implementation of a vaccine program has also been linked to improved child nutrition measures at the community level. A study from India found that on average there was a 22-25% reduction in stunting and a 15% reduction in weight-for-age deficit per child after rollout of its Universal Immunization Program. It is important to note that this study evaluated the impact of a vaccination program rather than the effect of vaccination in individual children. The authors describe that the vaccination program may have improved the primary care health infrastructure or resulted in increased maternal education and awareness of child nutrition and disease prevention. These collateral gains of implementing a vaccine program were also observed in an Indonesian study study of 24 communities, which found that children living in communities with higher overall levels of immunization were less likely to be malnourished as measured by how thin they were for their age.
These collateral gains of implementing a vaccine program were also observed in an Indonesian study of 24 communities, which found that children living in communities with higher overall levels of immunization were less likely to be malnourished as measured by how thin they were for their age.
According to a WHO report on global health risks, vaccines are part of a multi-pronged approach to reduce childhood underweight (along with nutritional interventions – such as micronutrient supplementation for children and women of child bearing age, and exclusive breastfeeding in infancy), which is the leading risk factor for death and disability in low income countries.1 By protecting children against common and sometimes deadly diseases, vaccines play a role in breaking the vicious cycle of infection and turning the tide on the hidden epidemic of undernutrition.
FOR ADDITIONAL INFORMATION:
1WHO. Global health risks: mortality and burden of disease attributable to selected major risks. 2009. Available at: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf.
2Bhutta ZA, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet 2013; 382: 452-477.
3RE Black, CG Victora, SP Walker, et al., the Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet (2013) published online June 6.
4WHO Media centre. Children: reducing mortality. 2017. http://www.who.int/mediacentre/factsheets/fs178/en/
5UNICEF, WHO, World Bank. Levels and trends in child malnutrition: UNICEF/ WHO/ World Bank Group joint child malnutrition estimates, key findings of the 2017 edition. 2017. Available at: http://www.who.int/nutgrowthdb/jme_brochoure2017.pdf?ua=1.
6WHO. Stunting. Accessed at http://www.who.int/mediacentre/infographic/nutrition/infographic-stunting.pdf?ua=1.
7Prendergast AJ. Malnutrition and vaccination in developing countries. Phil Trans R Soc B 2015; 370: 20140141.
8Katona P and Katona-Apte J. The interaction between nutrition and infection. CID 2008; 46(10): 1582-1588.
9S Horton, RH Steckel Global economic losses attributable to malnutrition 1990–2000 and projections to 2050. B Lombard (Ed.), appearing in: How much have global problems cost the world? A scorecard from 1900 to 2050, Cambridge University Press, Cambridge (2013)
From the VoICE Editors: This source was a working paper associated with the development think tank, The Copenhagen Consensus Center, which has been published in a 2013 Cambridge University Press book. Additional context and explanation of this paper may be found here: http://www.copenhagenconsensus.com/publication/scorecard-humanity-malnutrition-horton-steckel
10Black RE and the Maternal and Child Nutrition Study Group. Maternal and child nutrition: building momentum for impact. Lancet 2013; 382: 372-375.
11WHO. Rotavirus vaccines: WHO position paper—January 2013. WER 2013; 5(88); 49-64.
12Isanaka S, et al. Efficacy of a low-cost, heat-stable oral rotavirus vaccine in Niger. NEJM 2017; 376: 1121-1130.
13Cutts FT, et al. Efficacy of nine-valent pneumococcal conjugate vaccine against pneumonia and invasive pneumococcal disease in The Gambia: a randomised, double-blind, placebo-controlled trial. Lancet. 2005;365:1139-46.
14Madhi SA, et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. NEJM 2010; 362(4): 289-298.
15Watt JP, et al. Haemophilus influenza type b conjugate vaccine: review of observational data on long term vaccine impact to inform recommendations for vaccine schedules. 2012. Available at: http://www.who.int/immunization/sage/meetings/2012/november/5_Review_observational_data_long_term_vaccine_impact_recommendations_vaccine_schedules_Watt_J_et_al_2012.pdf.
