In February 2018, Angela Chang and colleagues released a widely publicized study in Health Affairs estimating the death and economic impoverishment (due to medical expenses) that could be averted in 41 low-income nations through the use of 10 vaccine antigens from 2016-2030. Here, the VoICE team brings you “New Research Cliff Notes”, where we provide a high-level explanation of this new study, important considerations, notes on interpretation and drivers of the study’s estimates.
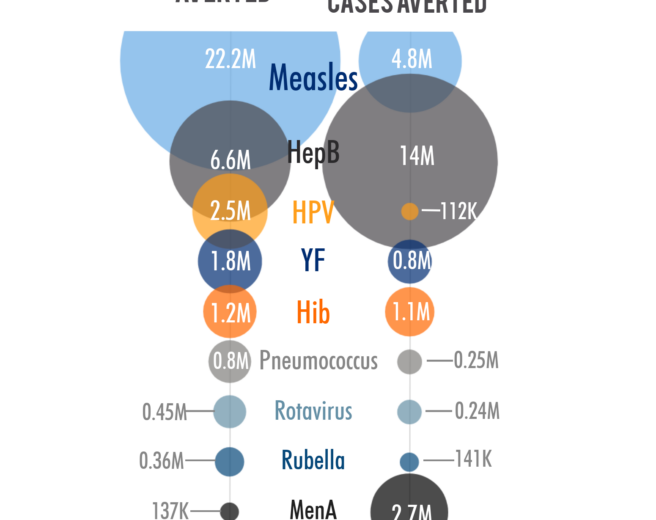
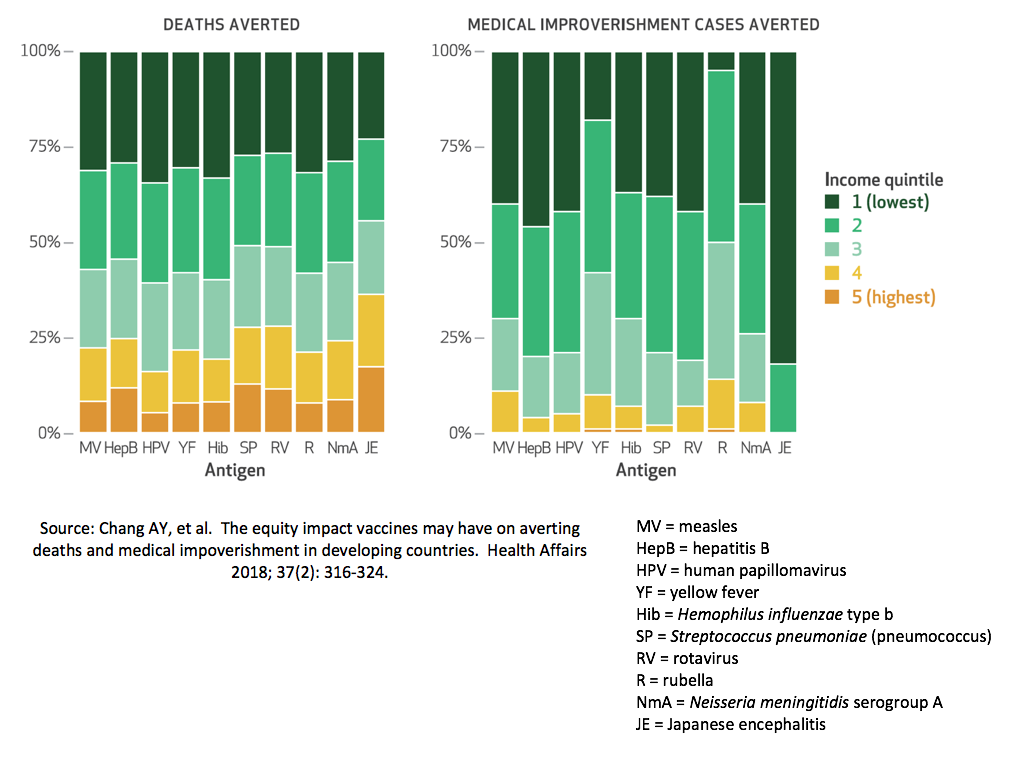
A pernicious cycle of poverty and ill health exist and vaccines can help to break this cycle. By preventing disease, vaccination also prevents the costs associated with disease treatment and thus helps to reduce the likelihood that households will fall into or remain in poverty. Within countries, greater benefits are observed among the poorest populations who often have higher risks of disease and death, reduced access to care, and are at significantly greater financial risk from medical expenses incurred to treat an episode of illness, as illustrated in Figure 1.
Figure 1: Drivers of health inequity and financial risk in low- vs high-income households
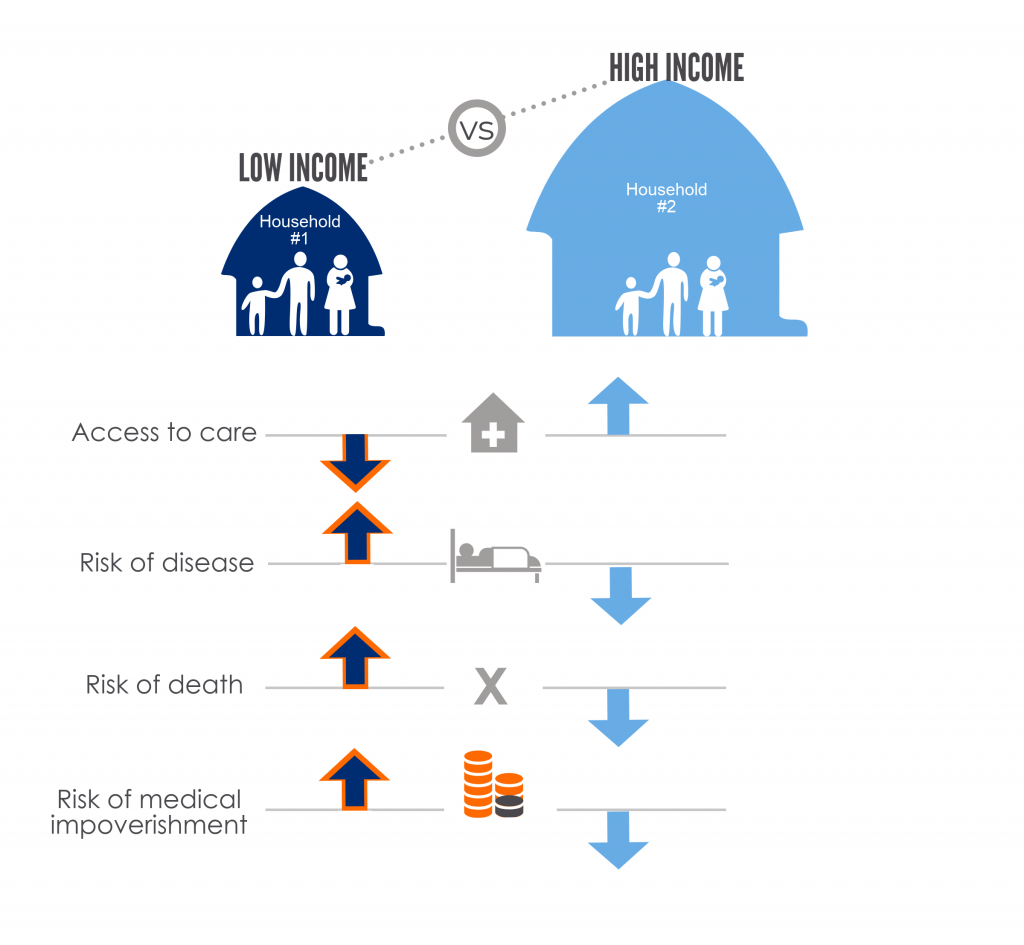
When children or adults become ill, families may have to use savings, sell property, or even take out loans to pay for their care. Additionally, their time spent away from domestic or paid work may impact negatively on their income. In short, an episode of illness can both increase expenses and reduce incoming finances, and thereby drive families into poverty. Figure 2 illustrates what can happen to a family living “paycheck-to-paycheck”, with limited or no savings and whose necessary expenses are roughly equivalent to their income.
Figure 2: The financial risk of unexpected medical expenses to a family living close to the poverty line
To what extent could vaccines impact this paradigm by preventing disease episodes leading to medical impoverishment? Recently, Angela Chang and fellow researchers have tried to estimate this, as well as to predict which people in low-income countries would reap the greatest health equity benefit and financial risk protection from vaccines. [Ref: Chang, et al. Health Affairs 2018]
The study: a look at the equity and poverty impact of vaccines
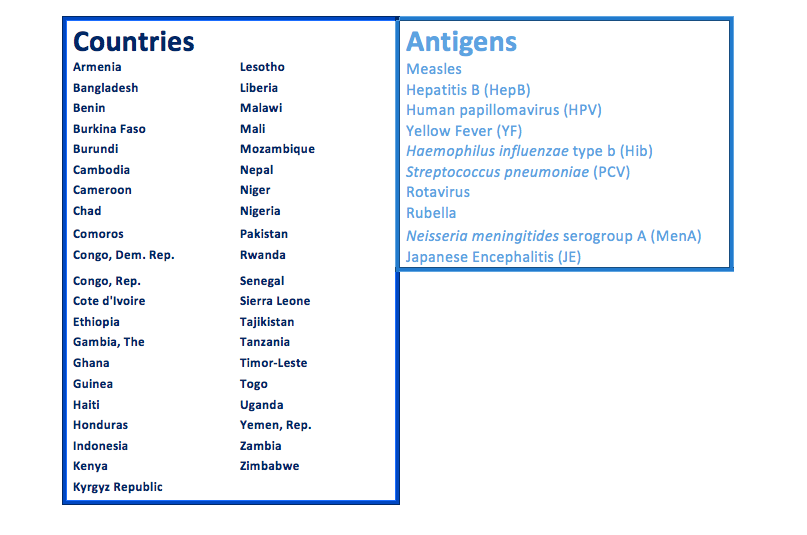
Chang and colleagues looked at the impact of 10 vaccine antigens in 41 low- and middle-income countries over the 15-year period of 2016 to 2030. (See Table 1 below) Using models to quantify the distribution of cases and deaths, the researchers compared the impact of these 10 antigens at expected coverage and efficacy levels, versus no vaccination. In this way, the authors could identify which vaccines should provide the largest benefits in terms of health gains, protection against financial risk, and equity.
Table 1: 41 countries and 10 antigens included in the equity and medical impoverishment analysis
What does it mean to have modeled data?
Models are mathematical equations that try to predict certain specified outputs that are difficult to empirically study based on inputted numbers. For example, you can estimate the number of disease cases in a population by using the incidence rate (that may be derived from a study in another population), and multiplying that by the number of people at risk of getting the disease in the population of interest.
Number of disease cases = new cases of disease per 100,000 persons x number of susceptible persons
Sometimes the inputs into a model are well-known, and sometimes there is a lot of uncertainty in the inputs used. In the latter case, that also means that the outputs of the models can vary a lot based on the model assumptions. For this reason, researchers should explain what assumptions they made to choose the inputs for their model. Often, modelers may also test different input values to see how variable the resulting estimates can be; this is called a sensitivity analysis.
Study findings: key drivers of the model
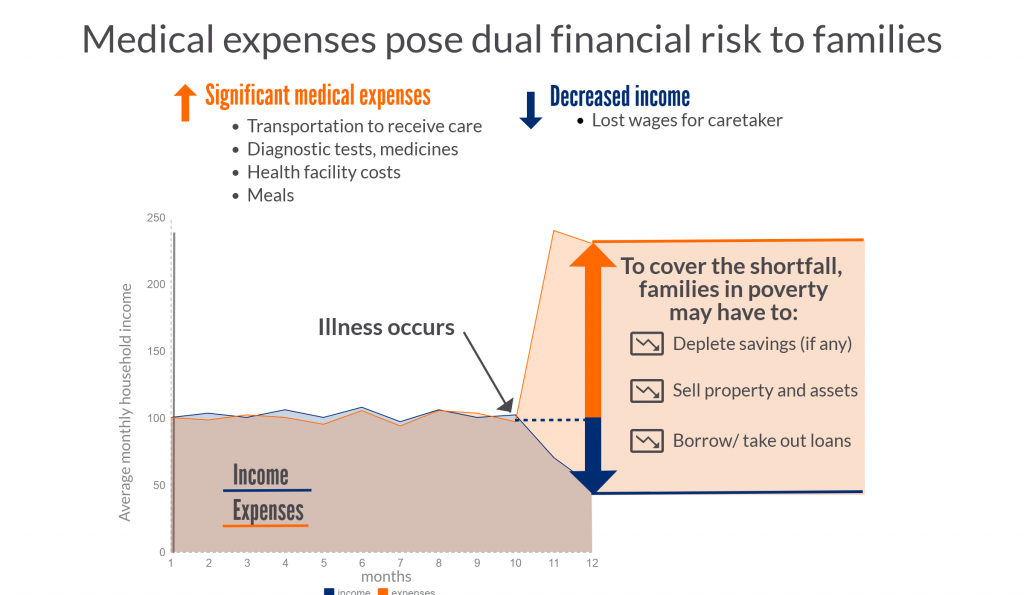
The model developed by Chang et al estimates that thirty-six million future deaths could be prevented by using the 10 vaccines during the period 2016-2030, compared to not using any of the vaccines. Measles accounted for 22 million deaths prevented, about 60% of the total deaths averted. There are several reasons why measles makes up such a large part of the mortality and medical impoverishment benefits, including: high, widespread coverage; measles infection is highly contagious and, in the absence of vaccination, would lead to significant outbreaks; measles has a relatively high mortality rate. (See Figure 3 below)
Medical impoverishment refers to the number of households that would be pushed below the poverty level due to the costs incurred from seeking, and paying for, treatment for a disease. The household poverty line was set at the World Bank level of $1.90 per day (2011 international dollars). Using these vaccines, researchers estimate that 24 million households that received immunizations between 2016-2030 would avoid falling below the poverty line. Hepatitis B and measles together account for about 80% of these cases.
It is important to note that in this study, those households that are already below the poverty line do not count towards the cases of medical impoverishment averted. However, these families would be further set back financially if they need to pay for medical care and would benefit significantly from the financial risk protection that immunization affords. That stark reality is that it is not uncommon for these families to make the hard decision not to seek care because they cannot afford to do so.
Figure 3: Drivers of deaths and cases of medical impoverishment averted through the use of 10 antigens in 41 countries, 2016-2030
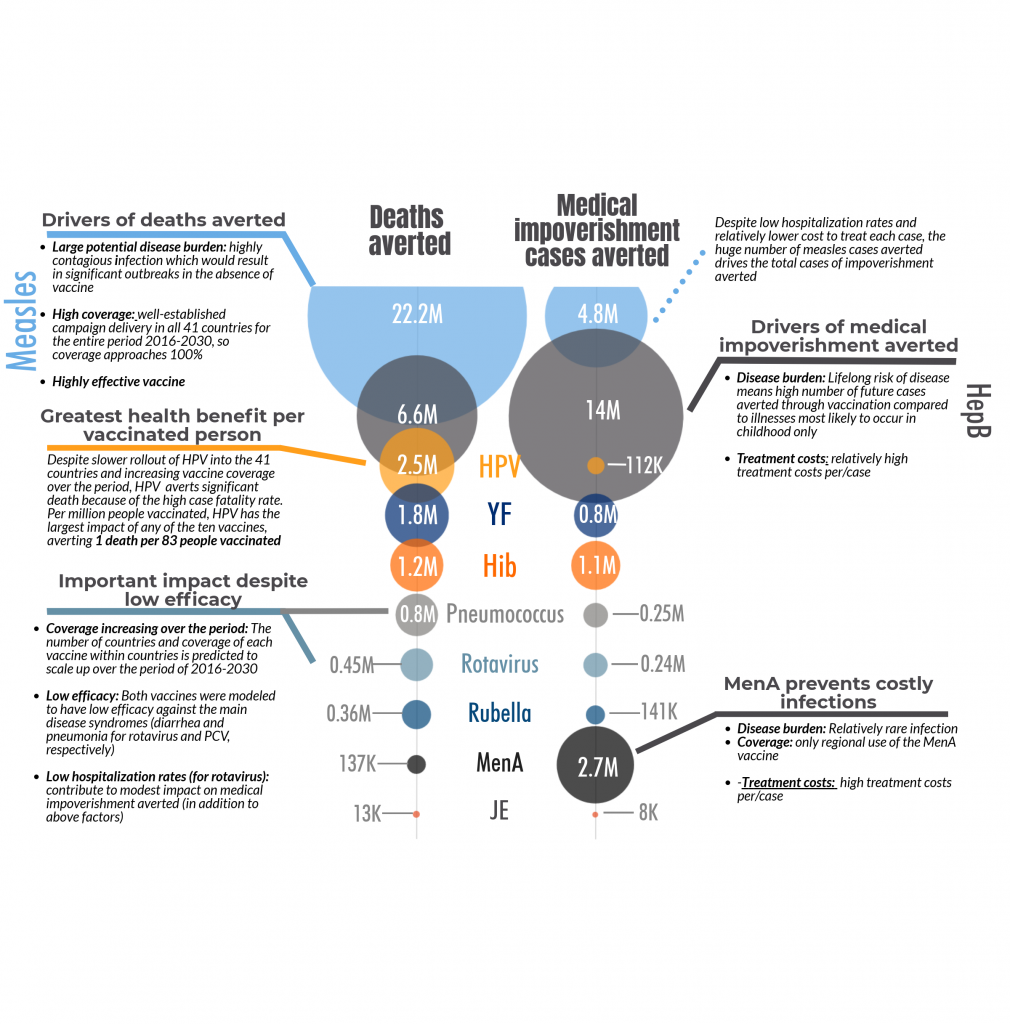
As you can see from the notes in Figure 3, certain key input variables drive the results. However, two antigens may have similar impact estimates but for significantly different reasons. For deaths averted the key variables considered were:
- Prevalence of risk factors for the disease by income level: for example, vitamin A deficiency or malnutrition, which are much more common in the poorest quintile than in the wealthiest
- Number of countries using the vaccine between 2016 and 2030, and year of introduction
- Expected vaccine coverage rate over time, in countries that have introduced a given vaccine
- Effectiveness of the vaccine in preventing disease
- Treatment coverage rate: how many people with the disease will seek medical care
- Risk of death among cases of disease (case fatality risk, which includes a measure of treatment effectiveness)
Disease impact of vaccines: the poor have more to gain
As seen in Figure 4 below, over half of all deaths averted for most diseases would come from those families in the lowest two wealth quintiles, the poorest 40% of households. People from these households are at higher risk of disease because they have a higher prevalence of risk factors (such as malnutrition or lack of sanitation) and poorer outcomes if they get sick. Also, because of the higher fertility rate, there are more people in the poorer income quintiles who are at risk of disease. So even though the poor have lower vaccine coverage rates in general, they have more to gain in terms of absolute numbers of averted deaths.
Illness-related poverty: who is at risk and what do the numbers mean?
For medical impoverishment, the most significant input variables for the model include:
- The number of disease cases or burden of the disease
- Care seeking behavior: how many people with the disease will seek medical care
- Household financial risk (i.e. how close the household is to the poverty line before seeking disease treatment – See Figure 2 above for an example scenario)
- Household expenses related to disease treatment, which can vary by:
- Severity of illness
- Length of hospital stay
- Cost of hospital stay per day
- Costs of tests and medications
- Additional household expenses related to treatment including
- Transportation costs to get to and from the clinic or hospital
- The lost wages for time away from work because of medical care
Figures 3 and 4, above, illustrate some of the ways of considering what drives the numbers of illness-related poverty, and how the numbers predicted can vary based on the disease and vaccine context.
Important to note…
- Those households that are already below the poverty line do not count towards the cases of medical impoverishment averted. The study evaluated how many people above the $1.90/day threshold would be pushed below that figure due to medical expenses, thus people already below the threshold are not counted. However, these already impoverished families would be pushed further into poverty if medical expenses were incurred, and would benefit significantly from the financial risk protection that immunization affords. That stark reality is that it is not uncommon for these families to make the hard decision not to seek care because they cannot afford to do so.
- The equity and poverty reduction impact analysis can be measured in four dimensions:
- burden of disease averted (e.g. deaths and cases of disease averted);
- financial risk protection afforded by vaccines (i.e. the protective effect of vaccines against household expenditures for disease treatment)
- transportation to health facility, productivity and wage losses
- equity (distributional consequences among population subgroups (e.g. income groups, subnational regions); and costs needed to sustain the vaccine policy
- Varying inputs to the model will also change the resulting estimates of deaths and medical impoverishment averted.
- Some model inputs may affect the estimates for deaths and medical impoverishment cases differently. For example, higher healthcare utilization rates lead to a lower predicted number of deaths averted—because fewer disease cases progress to death when more people access care – but also result in higher predicted cases of illness-related poverty averted as more people would incur treatment costs when they access care.
Finally, a few key points…
- Vaccination in low- and middle-income countries can substantially decrease child mortality but also prevent disease-related hospitalizations, health-related impoverishment, and bring significant financial risk protection to households.
- Within countries, greater benefit is expected among the poorest populations who often have higher risks of death, reduced access to effective care, and bear significant economic costs due to disease treatment.
- The total predicted number of cases of illness-related poverty averted—24 million—represents about 9% of people in low-income countries who are already impoverished. The use of these 10 vaccines prevents adding to the ranks of poverty by reducing disease burden and the associated—sometimes catastrophic—cost of care.
- Care should be taken in comparing the relative benefits of different vaccines/antigens because the context for each significantly influences the broader impact on health and financial risk.
- Each of the 10 vaccines evaluated had the greatest impact on deaths and medical impoverishment in the poorest 40% of households across these 41 countries.
