Evidence from several disciplines indicates that immunization has a broader role to play in lessening the impact of cancer than one might expect. While it may be obvious that the widespread and growing use of vaccines against Hepatitis B and human papilloma virus (HPV) is directly responsible for preventing a significant number of related cancers, immunization against a host of other diseases may indirectly help to prevent additional cancers while helping to protect the health of immune-compromised cancer patients considerably. Read on for a brief explanation of how vaccines can prevent cancer, protect cancer patients and more.
A selection of VoICE evidence in this issue
The direct benefits of preventing cancer-causing infections
HepB and liver cancer
Introduced in 1982, the hepatitis B vaccine was the first widely available vaccine to directly prevent cancer. More than 1 billion doses of HepB vaccine have been delivered, resulting in a significant reduction in the chronic liver infection that leads to cirrhosis or cancer in roughly a quarter of adults. The risk of HepB infection begins at birth – and lasts throughout a person’s life – which is why HepB is the first vaccine most children receive, often within hours of coming in to the world. In fact, 80-90% of children who are infected with HepB during the first year of life will go on to develop chronic liver disease, dramatically increasing their cancer risk.
HPV and cancer
A leading cause of death among women, cervical cancer took the lives of more than a quarter of a million women in 2012, 85% of whom were from low- or middle-income countries. Cervical cancer is caused by human papillomavirus (HPV), a common infection that can lead to abnormal cell growth and high-mortality cancers. Just two of the more than 100 strains of HPV are responsible for 70% of cervical cancers and precancerous lesions. Each of the three available HPV vaccines has been proven effective in preventing infection with high-risk strains of HPV and could protect against other forms of cancer caused by the virus. The exceedingly high mortality rate for cervical cancer (1 in 2 women will succumb to the disease) is due largely to the lack of access to early detection and treatment for women in much of the world, and reinforces the urgency of prevention through vaccination.
Additional benefits
HepB, Hib and polio vaccines
Some intriguing new evidence suggests that vaccines against HepB, Hib and polio may indirectly help to prevent the development of childhood cancers. Some scientists have suggested that early and robust stimulation of a child’s immune system – such as that afforded by vaccination – could help the body recognize and neutralize early tumors, thus decreasing the risk of developing certain childhood cancers such as leukemia. A study from the state of Texas in the US tested this idea and found that children born in counties with high coverage of HepB, polio and Hib vaccine were 33-42% less likely to develop a specific kind of leukemia than children born in counties with low vaccine coverage. Although only a small number of studies have demonstrated this indirect benefit of immunization on childhood cancers thus far, it is an exciting new area we will be following closely.
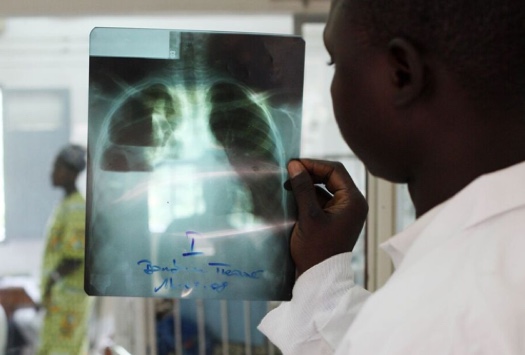
Protecting cancer patients and survivors from other infections
Cancer and cancer treatments can severely diminish the body’s capacity to fight infection, putting cancer patients and survivors at significantly greater risk of vaccine-preventable diseases and death from secondary infections. For example, a study of adults in the US found that invasive pneumococcal disease was more than 20 times more likely to occur in cancer patients than in cancer-naïve people. In a large study that followed survivors of childhood and early adult cancers for more than 5 years, researchers found a significantly higher rate of infections than in the siblings of these patients. Cancer survivors in this study were also 4 times more likely to die of infectious causes than their siblings. Pneumonia, a potentially vaccine-preventable infection, carried some of the highest increased risk to cancer patients, even more than 5 years after cancer diagnosis.
Survivors of pediatric and young-adult cancers must also be concerned about developing other forms of cancer later in life, some of which may be preventable through use of the HPV vaccine. A large study in the US found that longterm cancer survivors – both men and women – appeared to have a significantly increased risk of developing HPV-associated cancers and malignancies later in life. For these reasons, it is critical that cancer patients and survivors be vaccinated, and sometimes re-vaccinated, to ensure the greatest possible protection from additional infection.
Herd immunity in the general population is also an important protective firewall for cancer patients [1] weakened by the disease who may not yet have been vaccinated. Immune-suppressive treatments commonly used to treat some forms of cancer may erase the immunity a patient had already built up through previous vaccination and leave the immune system too weak to tolerate immunization.
The economic benefits of cancer prevention are substantial
Preventing cancer has significant economic implications, and vaccines that help prevent cancer carry a significant return on investment in a variety of settings.
Hep B: Economic benefits
In terms of economic benefits, HepB vaccine carries a high economic return on investment, due in part to the sustained risk of infection across the lifespan. Health economists have estimated that during the decade 2011-2020, the use of this vaccine in the world’s poorest countries will have a return of over nine times its cost, thanks to the widespread use and high effectiveness of HepB Vaccine.
HPV: Health System and economic benefits
HPV vaccine is recommended to be given to girls in early adolescence (as opposed to most other childhood vaccines which are given during the first few years of life), which has resulted in some unique opportunities to expand delivery of other health services to this age group – even those not receiving the vaccine – and to form new collaborations between agencies that may help strengthen health programs overall.
Despite gradual uptake of HPV vaccine among the world’s poorest countries, health economists have estimated a 3-fold return on investment from the use of HPV vaccine in these countries during this decade (2011-2020). Averting the premature death of women through prevention of cervical and other HPV-related cancers increases overall productivity and would prevent destabilization of families and communities.
[1] High vaccine coverage in the general population significantly reduces the chance that an infectious agent is transmitted to others, significantly reducing the risk that an unvaccinated person will be exposed and infected. This phenomenon is called herd immunity.
