“The climate crisis threatens to undo the last fifty years of progress in development, global health, and poverty reduction, and to further widen existing health inequalities between and within populations.”1
With July 2023 confirmed as the hottest month on record2, the impacts of climate change are becoming impossible to ignore. In addition to rising temperatures, climate change is also responsible for increasingly frequent extreme weather events like intense storms, catastrophic floods, and record-breaking heat waves. A growing body of evidence suggests that the consequences of climate change pose a major threat not only to the planet, but also to human health.
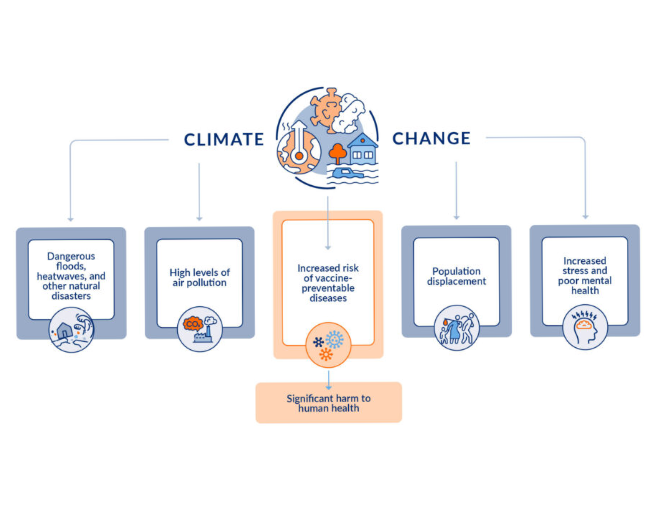
Altogether, climate change is expected to cause around 250,000 excess deaths per year between 2030 and 2050 due to malnutrition, malaria, diarrhea, and heat stress alone1. In addition to the excess mortality that is directly attributable to natural disasters, the wide-ranging effects of climate change can also indirectly contribute to illness and death through several pathways. Warm, dry conditions trigger more frequent wildfires3, which in turn contribute to dangerous levels of air pollution4. The stress of living through an extreme weather event and the resulting loss of critical resources has been linked with poor mental health5. Furthermore, climate change is expected to increase the prevalence of several vaccine-preventable diseases, such as malaria, cholera, and typhoid, thanks to the expansion of mosquito habitats, scarcity of clean water, and disruptions to routine immunization, among others6.
No one is safe from the effects of climate change, but its impact reflects deep inequities. Already marginalized communities – particularly those in developing countries – will be disproportionately affected due to existing health disparities and insufficient health system infrastructure7. To minimize climate change-related health impacts, equitable access to vaccines must be a priority, especially for those who will be most affected in the years to come.
Rising Temperatures Increase Disease Transmission
In August 2023, global temperatures were approximately 1.5°C above preindustrial levels8. In addition to the illnesses and deaths caused directly by these dangerously high temperatures, such as those related to heat stroke9, collateral effects also include increased transmission of a number of vaccine-preventable diseases.
Warmer winters and hotter summers are expected to increase the evaporation of water sources, endangering the availability of safe, clean water and increasing the risk of diarrheal diseases10. This includes cholera, which has recently seen a global surge: The WHO reported 472,697 cases of cholera in 2022, nearly double the number reported in 202111. Rising temperatures reduce the availability of high-quality crops12, threatening food security and leading to dangerous malnutrition that weakens a child’s immune system and increases the risk of infectious disease.
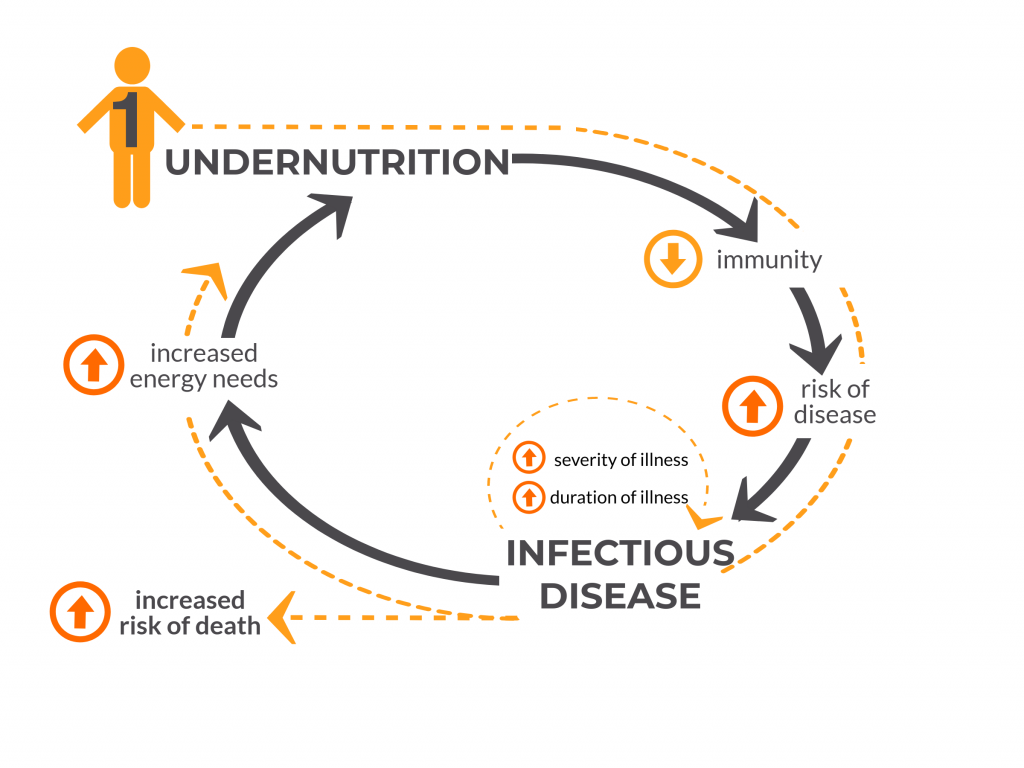
An analysis of 14 countries in sub-Saharan Africa13 demonstrated that for every 1°C increase in average maximum temperature, the prevalence of diarrhea increased by about 1%. The reasons for this association are not entirely clear, but researchers point to the impact of heat on the growth and survival of diarrhea-causing bacteria, as well as the potential for heat-related changes in hygiene or food storage. This increase in disease burden may significantly impact vulnerable populations, especially young children, as diarrhea is currently the second most deadly infectious disease worldwide and kills over 480,000 children under 5 each year14. We already have the means to prevent rotavirus infection, the leading cause of diarrhea-related mortality among children around the world – a 2018 analysis estimated that if 100% of children globally had access to rotavirus vaccination, more than 83,000 child deaths could be prevented in a single year15 – yet millions of children around the world are still unprotected against this disease16. As global temperatures continue to rise, efforts to increase access to lifesaving rotavirus vaccines will remain critical.
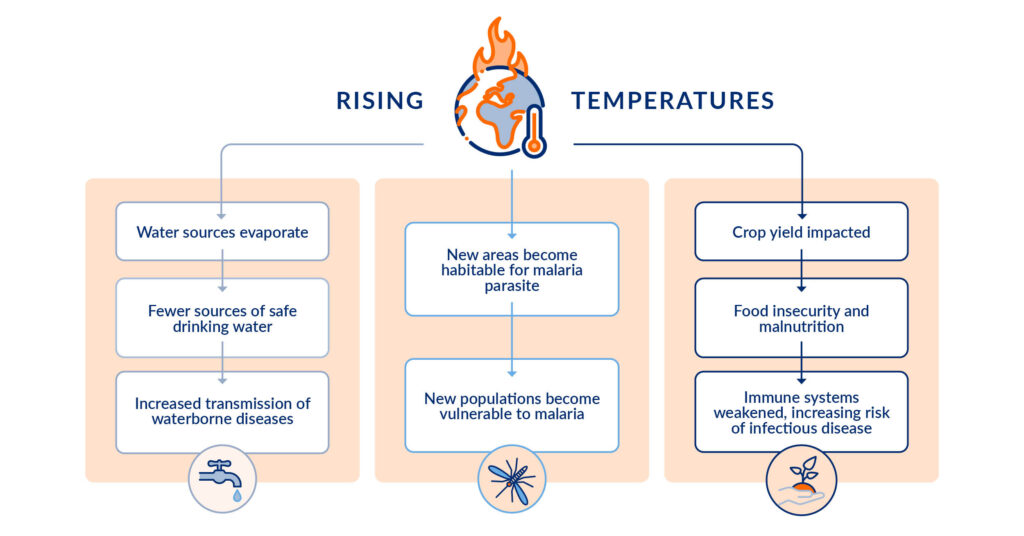
Temperature changes are also expected to impact transmission of vector-borne diseases, including malaria. About 80% of the world’s population lives in a region that is at risk of at least one vector-borne disease17, and this number could grow as temperatures continue to rise. The malaria parasite develops more quickly at higher temperatures, increasing the chance that a mosquito will survive long enough to transmit the disease18. Additionally, areas that are presently too cold for malaria transmission may warm up enough to allow malaria parasites to survive, exposing new populations to this deadly disease. One recent analysis estimated that around 1.4 billion additional people will be at risk of malaria and dengue in urban areas in Africa and southeast Asia due to changes in climate19. On the other hand, areas where malaria is currently being transmitted may become too warm, which could actually decrease incidence of the disease. Controlling malaria is already complex, but additional climate-related factors such as temperature, rainfall, and humidity may be important considerations for preventing outbreaks.
The Dangerous Consequences of Floods and Droughts
“Climate change is exacerbating both water scarcity and water-related hazards (such as floods and droughts), as rising temperatures disrupt precipitation patterns and the entire water cycle.”20
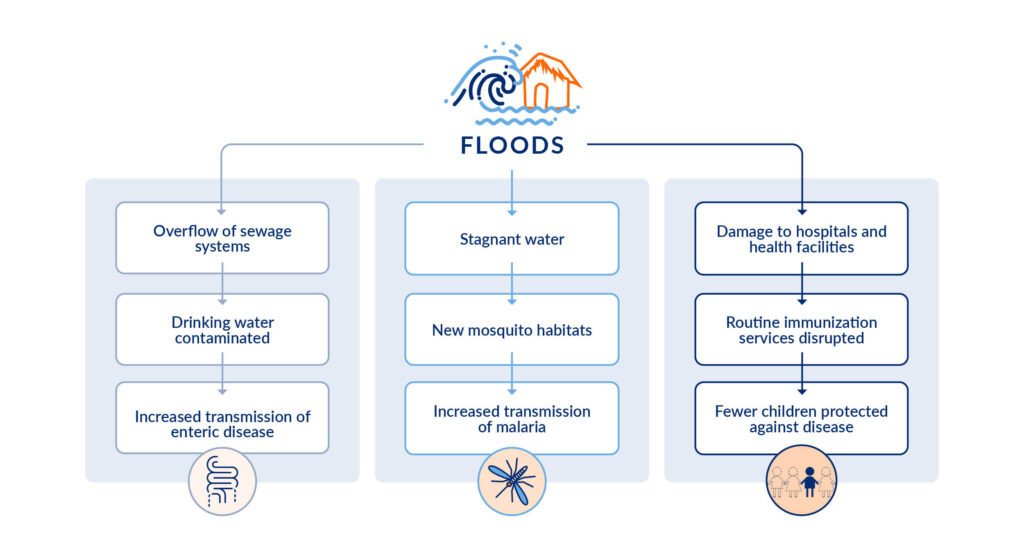
Between 2001–2018, nearly two-thirds of natural disasters were water-related21, and floods and droughts are only expected to become more intense and more frequent as climate change worsens. These events threaten the availability of safe drinking water and can increase transmission of enteric diseases. For example, both droughts and floods have been found to be significantly associated with cholera outbreaks in sub-Saharan Africa22; in this region, a cholera outbreak can be expected in 1 out of every 3 droughts. During a drought, communities searching for water can be forcibly displaced, often to overcrowded refugee camps with poor sanitation and limited access to cooking tools, increasing the risk of contamination and disease transmission.
Conversely, floodwater can overflow sewage systems and contaminate drinking water23. This contaminated water can also destroy WASH facilities, further putting communities at risk of disease transmission. Additionally, the heavy rainfall and stagnant water associated with flooding can create new mosquito habitats and increase breeding. In 2007, for example, areas in China impacted by flooding saw significantly higher numbers of cases of both malaria and diarrhea than non-flood-affected areas24. Lastly, floods and other disasters can seriously disrupt the delivery of health services, including vaccination25. Not only can flood water damage hospitals and health clinics, making it difficult or even impossible to provide routine immunization services, but it can also block roads, potentially leading to supply chain gaps that can impact the availability of vaccines and other critical medical supplies.
Disproportionate Impact to Disadvantaged Populations
Every year, approximately 21.5 million people around the world26 are forced to leave their homes due to climate-related disasters like floods, storms, wildfires, and extreme temperatures, and this number is only expected to continue growing27. These individuals are often referred to as “climate refugees”, though this includes those internally displaced within their own countries as well as those pushed across borders to seek safety. Climate-related displacement disproportionately impacts those living in low-resource settings, who are less able to prepare for and withstand natural disasters. Even within low- and middle-income countries (LMICs), climate change is more likely to impact those who are already most deprived. According to an analysis in Pakistan, the regions with worse socioeconomic conditions are also the most vulnerable to climate change28. The same analysis also found that some regions which should be most exposed to climate change due to their precipitation and temperature patterns are actually less vulnerable, most likely because their populations have higher socioeconomic status and thus a higher capacity to adapt, suggesting that strengthening a community’s resilience is one potential solution to fight the impacts of climate change.
In addition to equity considerations, forced migration can also lead to increased risks of vaccine-preventable disease outbreaks. Disruption to health services, malnutrition, overcrowded settlements, and insufficient sanitation resources all contribute to infectious diseases, such as pneumonia and diarrhea, which are the leading causes of death during humanitarian emergencies29. Vaccination programs that target measles, S. pneumoniae, H. influenzae type-b, and rotavirus have already been recognized as critical tools for reducing the health impacts of complex humanitarian emergencies.
Mitigating the Impact of Climate Change with Vaccines
At this point, the impact of climate change is inevitable, but there are steps we can take to mitigate its effects on human health. We must strengthen efforts to increase access to vaccines for diseases that will become more prevalent as extreme weather events continue, prioritizing disadvantaged communities that will be hardest hit by climate-related disasters. Beyond vaccine introduction, we must work to make sure that adequate supplies are made available to those who need them most. For example, millions of doses of life-saving malaria vaccines30 are being rolled out in Africa over the next two years, but there is still significant work to be done to meet the global demand for these vaccines and to ensure that LMICs can afford them31. Similarly, the global supply of oral cholera vaccine (OCV) is currently unable to meet the needs of more and more frequent cholera outbreaks and must be allocated equitably32.
Over the last decade, enormous victories have been won in protecting children from preventable illnesses. As climate change has been recognized as a serious threat to public health, policymakers must take decisive action now to safeguard vulnerable populations from potentially catastrophic infectious diseases and counteract immunization backsliding.
Additional Reading
Will the Earth’s changing climate make TB spread faster? [Bhekisisa Centre for Health Journalism]
Children displaced in a changing climate: Preparing for a future that’s already underway [UNICEF]
Vaccines for a sustainable planet [Science Translational Medicine]
References
- World Health Organization. Climate change and health. Updated 30 October 2021. Accessed September 28, 2023. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
- World Meteorological Organization. July 2023 confirmed as hottest month on record. 14 August 2023. https://public.wmo.int/en/media/news/july-2023-confirmed-hottest-month-record
- National Oceanic and Atmospheric Administration. Wildfire climate connection. Updated 24 July 2023. Accessed September 28, 2023. https://www.noaa.gov/noaa-wildfire/wildfire-climate-connection
- World Health Organization. Wildfires. Accessed September 28, 2023. https://www.who.int/health-topics/wildfires
- Cianconi P, Betro S, Janiri L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Frontiers in Psychiatry. Mar 6 2020;11(74). doi:10.3389/fpsyt.2020.00074
- Joi P. Five key links between climate change and health. VaccinesWork blog. 2023. https://www.gavi.org/vaccineswork/five-key-links-between-climate-change-and-health
- Byers E, Gidden M, Leclere D, et al. Global exposure and vulnerability to multi-sector development and climate change hotspots. Environmental Research Letters. 31 May 2018. doi:10.1088/1748-9326/aabf45
- World Meteorological Organization. Earth had hottest three-month period on record, with unprecedented sea surface temperatures and much extreme weather. 6 September 2023, 2023. https://public.wmo.int/en/media/press-release/earth-had-hottest-three-month-period-record-unprecedented-sea-surface
- World Health Organization. Heatwaves. Accessed September 28, 2023. https://www.who.int/health-topics/heatwaves
- International Federation of Red Cross and Red Crescent Societies, 2021. Climate Change Impacts on Health: Malawi Assessment. April 2021.
- World Health Organization. Weekly Epidemiological Record. Vol. 38. 2023:431-452. 22 September 2023.
- Zhao C, Liu B, Piao S, et al. Temperature increase reduces global yields of major crops in four independent estimates. Proceedings of the National Academy of Sciences. 2017;114(35):9326-9331. doi:10.1073/pnas.1701762114
- Bandyopadhyay S, Kanji S, Wang L. The impact of rainfall and temperature variation on diarrheal prevalence in Sub-Saharan Africa. Applied Geography. April 2012;33:63-72. doi:10.1016/j.apgeog.2011.07.017
- International Vaccine Access Center (IVAC), Johns Hopkins Bloomberg School of Public Health. (2022). Pneumonia and Diarrhea Progress Report 2022.
- Troeger C, Khalil IA, Rao PC, et al. (2018). Rotavirus vaccination and the global burden of rotavirus diarrhea among children younger than 5 years. JAMA Pediatrics. Oct 2018;172(10). doi: 10.1001/jamapediatrics.2018.1960
- International Vaccine Access Center (IVAC), Johns Hopkins Bloomberg School of Public Health. VIEW-hub. www.view-hub.org. Accessed 10/19/2023.
- Alonso P, Engels D, Reeder J. Renewed push to strengthen vector control globally. The Lancet. June 10 2017;389(10086):2270-2271. doi:10.1016/S0140-6736(17)31376-4
- Agyekum T, Botwe P, Arko-Mensah J, et al. A Systematic Review of the Effects of Temperature on Anopheles Mosquito Development and Survival: Implications for Malaria Control in a Future Warmer Climate. International Journal of Environmental Research and Public Health. 7 July 2021;18(14).doi:10.3390/ijerph18147255
- Colon-Gonzalez FJ, Sewe MO, Tompkins AM, et al. Projecting the risk of mosquito-borne diseases in a warmer and more populated world: a multi-model, multi-scenario intercomparison modelling study. The Lancet Planetary Health. July 2021;5(7):E404-E414. doi:10.1016/S2542-5196(21)00132-7
- United Nations. Water – at the center of the climate crisis. Accessed September 28, 2023. https://www.un.org/en/climatechange/science/climate-issues/water?gclid=CjwKCAjw3oqoBhAjEiwA_UaLtjFAZ_AFhkgP6lr0YAg7vlwTwZwUbsZa9T-pBajg0zu2QyOFKT8CpBoC3RIQAvD_BwE
- UNICEF. Water and the global climate crisis: 10 things you should know. Updated 2 March 2023. https://www.unicef.org/stories/water-and-climate-change-10-things-you-should-know
- Rieckmann A, Tamason CC, Gurley ES, et al. Exploring Droughts and Floods and Their Association with Cholera Outbreaks in Sub-Saharan Africa: A Register-Based Ecological Study from 1990 to 2010. The American Journal of Tropical Medicine and Hygiene. 2018;98(5):1269-1274. doi:10.4269/ajtmh.17-0778
- ten Veldhuis JAE, Clemens FHL, Sterk G, et al. Microbial risks associated with exposure to pathogens in contaminated urban flood water. Water Research. May 2010;44(9):2910-2918. doi:10.1016/j.watres.2010.02.009
- Gao L, Zhang Y, Ding G, et al. Identifying Flood-Related Infectious Diseases in Anhui Province, China: A Spatial and Temporal Analysis. The American Journal of Tropical Medicine and Hygiene. 2016;94(4):741-749. doi:10.4269/ajtmh.15-0338
- Pradhan NA, Najmi R, Fatmi Z. District health systems capacity to maintain healthcare service delivery in Pakistan during floods: A qualitative study. International Journal of Disaster Risk Reduction. August 2022;78. doi:10.1016/j.ijdrr.2022.103092
- UNHCR. Frequently asked questions on climate change and disaster displacement. Updated 6 November 2016. Accessed September 28, 2023. https://www.unhcr.org/uk/news/stories/frequently-asked-questions-climate-change-and-disaster-displacement
- Institute for Economics & Peace. Over one billion people at threat of being displaced by 2050 due to environmental change, conflict and civil unrest. September 9, 2020.
- Malik SM, Awan H, Khan N. Mapping vulnerability to climate change and its repercussions on human health in Pakistan. Globalization and Health. 2012;8(31). doi:10.1186/1744-8603-8-31
- Close RM, Pearson C, Cohn J. Vaccine-preventable disease and the under-utilization of immunizations in complex humanitarian emergencies. Vaccine. 2016;34(39):4649-4655. doi:10.1016/j.vaccine.2016.08.025
- World Health Organization. 18 million doses of first-ever malaria vaccine allocated to 12 African countries for 2023–2025: Gavi, WHO and UNICEF. 5 July 2023. https://www.who.int/news/item/05-07-2023-18-million-doses-of-first-ever-malaria-vaccine-allocated-to-12-african-countries-for-2023-2025–gavi–who-and-unicef
- Gavi, the Vaccine Alliance. Gavi outlines plans to build sustainable supply of malaria vaccines. 25 April 2023. https://www.gavi.org/news/media-room/gavi-outlines-plans-build-sustainable-supply-malaria-vaccines
- Gavi, the Vaccine Alliance. Global vaccine alliance outlines path to sustainable cholera vaccine supply. 22 May 2023. https://www.gavi.org/news/media-room/global-vaccine-alliance-outlines-path-sustainable-cholera-vaccine-supply
