December 12th is worldwide Universal Health Coverage (UHC) day! Although exceedingly complex in its implementation, the concept behind UHC is simple: All people should benefit from quality health services, medicines and vaccinations, and no one should be put in financial peril to do so. In recognition of UHC Day 2018, the VoICE team brings you a brief look at the interplay between coverage of immunization and other basic health interventions, and the important role of immunization in protecting against financial risk – both within the context of the Sustainable Development Goal Target for UHC.
A selection of VoICE evidence in this issue
Hinman, A.R., and McKinlay, M.A. 2015. Immunization equity. Vaccine. 33(2015).
Key Points
- Achieving universal coverage of basic health services will require strengthening and expanding current health systems AND new approaches to reaching those who still cannot or do not access health services.
- The reach of immunization delivery programs can be leveraged to provide other basic services – and increase financial efficiency of health systems – and the reverse is also true: the delivery of other interventions can help to increase the uptake of vaccines.
- Achievement of UHC will positively contribute to at least six of the 17 Sustainable Development Goals.
- Immunization can contribute significantly to achieving financial risk protection against health costs.
Universal Health Coverage and the Sustainable Development Goals
December 12th is worldwide Universal Health Coverage (UHC) day! The aim of drawing attention to this day is to shine the global spotlight on the gaps in achieving health as a human right. Although exceedingly complex in its implementation, the concept behind UHC is simple: All people should benefit from quality health services, medicines and vaccinations, and no one should be put in financial peril to do so.
In 2015, 193 United Nations Member States committed to an ambitious set of 17 “Sustainable Development Goals” (SDGs) by 2030. The right to health not only figures prominently as a goal in and of itself – SDG3 is to “Ensure healthy lives and promote well-being for all at all ages” – but is also fundamentally intertwined with goals related to equity, poverty, economic growth and inclusion. (See Figure 1.)
Figure 1: The interrelatedness of Universal Health Coverage with other Sustainable Development Goals, and the importance of health systems strengthening.
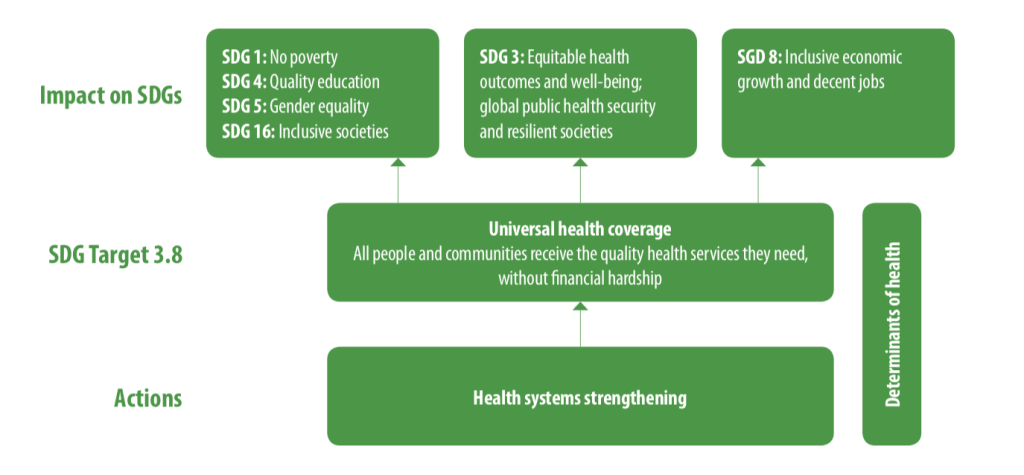
Embodied in the 8th Target of SDG3 (SDG 3.8), the pursuit of UHC is supported by the twin indicators of 1) coverage of essential services (including immunization), and 2) financial risk protection from the incurrence of economically burdensome health costs. In recognition of UHC Day 2018, the VoICE team brings you a brief look at the interplay between coverage of immunization and other basic health interventions, and the important role of immunization in protecting against financial risk – both within the context of SDG 3.8.
Building on coverage of vaccines gives UHC a head start, but there is more to do
Equity is at the heart of the Sustainable Development Goal target 3.8, which seeks to achieve universal health coverage and financial risk protection for all. The coverage indicator for the achievement of UHC tracks the coverage of 14 “tracer interventions”, which together serve as a barometer for access to basic health services. Access to immunization is tracked through the coverage of the third dose of DTP3, one of four maternal and child health tracer interventions. Although DTP3 coverage is evidence of the fact that immunization is one of the most widely available and equitably distributed interventions worldwide, several other important vaccines lag behind the 85% coverage of DTP3 worldwide in 2017.
Specific vaccines notwithstanding, high coverage with some vaccines such as DTP make immunization programs a critical backbone of any universal health coverage strategy. Routine and campaign-based immunization programs reach some children in remote or poverty stricken areas whose families have little other connection to the health system, and as such, offer opportunities to provide additional basic health care services to children and their families, especially interventions associated with maternal and child health. See Figure 2 for some highlights from VoICE of the opportunities for mutual reinforcement between immunization and other programs.
Figure 2: Examples of the integration of immunization and other health services.

Vitamin A distribution integrated with polio vaccine campaigns led to increased VitA coverage in several African countries.

Delivery of HPV vaccine to school-age girls in Rwanda provided an opportunity to offer school-age boys a variety of health services at the same time.

The timing of childhood immunizations could be harnessed to deliver a range of early childhood development interventions such as newborn hearing screening, sickle cell screening, treatment and surveillance, maternal education around key newborn care issues such as jaundice, and tracking early signs of poor growth and nutrition.
Despite the relatively high coverage globally of some vaccines, other critical vaccines have reached only a small fraction of the world’s children. Fully 15% of the world’s children are not reached at all by immunization – a gap whose distribution carries significant inequity – so vaccine coverage successes are very much tied to the achievement of UHC goals and targets for other health services.
The achievement of UHC targets will, however, require significant reform and expansion of existing health systems to address challenges such as missed opportunities to integrate services. For example, a recent study in 14 low- and middle-income countries found an exceedingly high rate of missed opportunities to vaccinate in 8 of the 14 countries, despite families coming into contact with the health system. For these countries, children failed to be vaccinated more than 50% of the time, despite they or their mother having received at least one of 5 other basic health interventions provided through the health system. Additionally, for the millions of families not reached at all by current health systems, barriers may include socio-cultural factors, in addition to geography, education, poverty, etc.
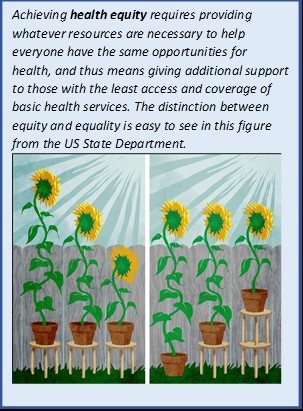
For these families and others with inadequate health services, a truly equity-driven approach is needed. That is, governments, partners, health-providers, and systems will need find ways to provide whatever additional support is needed to help them catch up, not just make the same resources available to everyone.
For families, financial barriers to immunization are relatively low, but health and economic returns are high
The second indicator of the universal health coverage target acknowledges that the costs associated with health care – both preventative services and treatment for illness – are a significant barrier for hundreds of millions of people around the world. These costs prevent some people from even trying to access health services, and for those who do seek care they cannot afford, the financial burden of these services can have significant, negative and lasting economic impact. The provision of a basic package of preventative services, including immunization, would thus create a positive, reinforcing cycle of increased health-seeking behavior and improved financial stability for individuals, families and economies.
Immunization is a critical element to success for two reasons. First, thanks to global institutions such as Gavi and UNICEF, immunization is free of charge for a large proportion of families in the world’s middle and low-income nations and financial barriers to access are thus relatively low. However, not all crucial vaccines are yet available through national immunization programs in every country. In some places, lifesaving vaccines against disease such as pneumococcal disease are only available through the private market, carrying a price tag far too high for many families to access. And, as mentioned above, sociocultural factors and other issues are significant drivers of gaps in vaccine coverage and these must be addressed carefully and concertedly.
The second reason immunization is critical to meeting the financial risk protection targets of UHC is much more obvious: the widespread use of vaccines has the power to avert significant costs associated with treatment of infections. The huge economic burden of these infections stems from the costs associated with treating relatively low-cost but frequently occurring infections and complicated infections such as meningitis which are rare but very expensive to treat. These vaccine-preventable episodes of illness are responsible for a large number of families being pushed into poverty each year.
Visit the VoICE tool to find out more about how vaccines can help people avoid economic impoverishment from medical costs. Read our feature on medical impoverishment averted through immunization in 41 low-income nations.

The hurdles that remain are high, but health for all awaits on the other side
The road to UHC will be fraught with risk and will require creative new ideas for reaching the unreached. For one, we must ensure that whatever systems are put in place to expand access to basic health interventions will not inadvertently damage immunization coverage, but will reinforce progress that has been made in expanding immunization coverage.
It is also clear that the achievement of UHC goals by 2030, or by any time, will require us to not only expand and improve upon the health systems that already exist, but also to change our approach to these imperfect health systems. Those families who receive no basic health services are called “hard to reach” for a reason. The challenge in devising a system flexible and comprehensive enough to reach everyone is very real, and very worthwhile.

