Despite tremendous global progress, diarrhea remains the second leading infectious cause of under-5 deaths, taking a child’s life almost every minute. Although diarrhea can seem like a common, simple childhood ailment in many places, a single episode of diarrhea can be serious, even deadly, and have severe economic implications for families and communities. Advocates play a critical role in ensuring evidence-based diarrhea prevention and control programs and policies are a top priority globally and in the countries where this disease is most prolific.
A selection of VoICE evidence in this issue
How preventing diarrhea can protect children, families, communities, and health systems
Despite tremendous global progress, diarrhea remains the second leading infectious cause of under-5 deaths, taking a child’s life almost every minute.[1],[2] Although diarrhea can seem like a common, simple childhood ailment, in many places a single episode of diarrhea can be serious, even deadly, and have severe economic implications for families and communities.
- Repeated, prolonged diarrhea can have lasting – but sometimes overlooked – impacts on child health and development.
- Treating diarrhea can be costly to families and health systems, and treatment costs can even push some families into poverty.
- Rotavirus causes approximately one third of diarrhea deaths, and is only adequately preventable via vaccination – water, sanitation, and hygiene interventions that work to prevent other types of diarrhea don’t work to prevent rotavirus.
- Cholera vaccination is used to stop endemic cholera and respond to cholera outbreaks, which are common in humanitarian emergency settings.
Advocates play a critical role in ensuring evidence-based diarrhea prevention and control programs and policies are a top priority globally and in the countries where the outcomes of diarrheal diseases are most devastating.
The burden of diarrhea globally
Each year, there are an estimated 1 billion episodes of diarrhea with approximately 500,000 deaths in children under five years of age.[1],[2] WHO estimates that children in low- and middle-income countries each have approximately three episodes of diarrhea a year.[3] Although improvements have been made in our efforts to stop diarrhea deaths, we still have far too many episodes: since 1990, the number of diarrhea deaths has decreased by 65%, but the number of new diarrhea episodes has decreased by only 24%.[4] This burden is disproportionally concentrated in low- and middle-income countries, with over half of the diarrheal deaths occurring in sub-Saharan Africa – a low-resource setting where progress is slowest.[5]
The impact of diarrhea on children
Each episode of diarrhea deprives a child of nutrition necessary for growth and contributes to malnutrition, making these children more vulnerable to diarrhea yet less able to fight it.[3] After an episode of diarrhea, children grow less in length than children who did not have diarrhea. When a child has repeated episodes of diarrhea, it can lead to chronic malnutrition and stunting, which in turn is associated with poor functional outcomes such as impaired cognitive development. Prolonged and frequent episodes of diarrhea in young children under the age of two affects them in later childhood and adolescence by leading to delays in school readiness and poor performance in school, as compared to their peers.
Episodes of diarrhea can exacerbate underlying undernutrition and can impair immunity hampering the ability to fight diseases such as pneumonia.[6] During diarrheal episodes, children can lose Vitamin A and zinc, which may predispose some children to pneumonia. In addition, children with more frequent episodes of diarrhea are more likely have chronic health issues later in life, like high blood pressure, which are taxing on both families and health systems.
Tools to defeat diarrhea
Aids to Help Protect and Prevent diarrhea disease and deaths
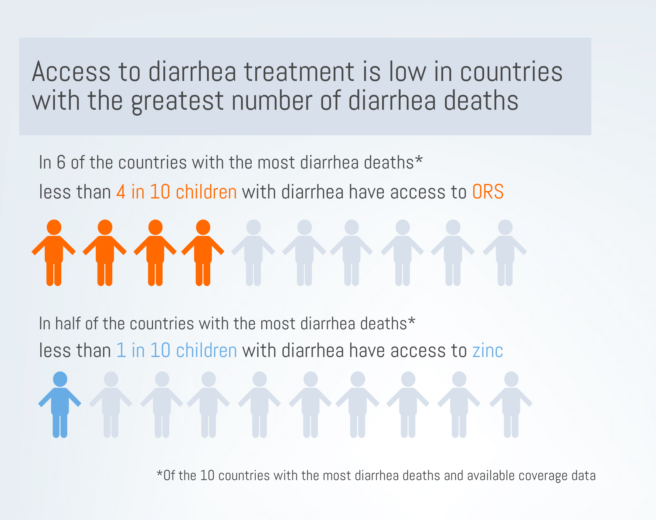
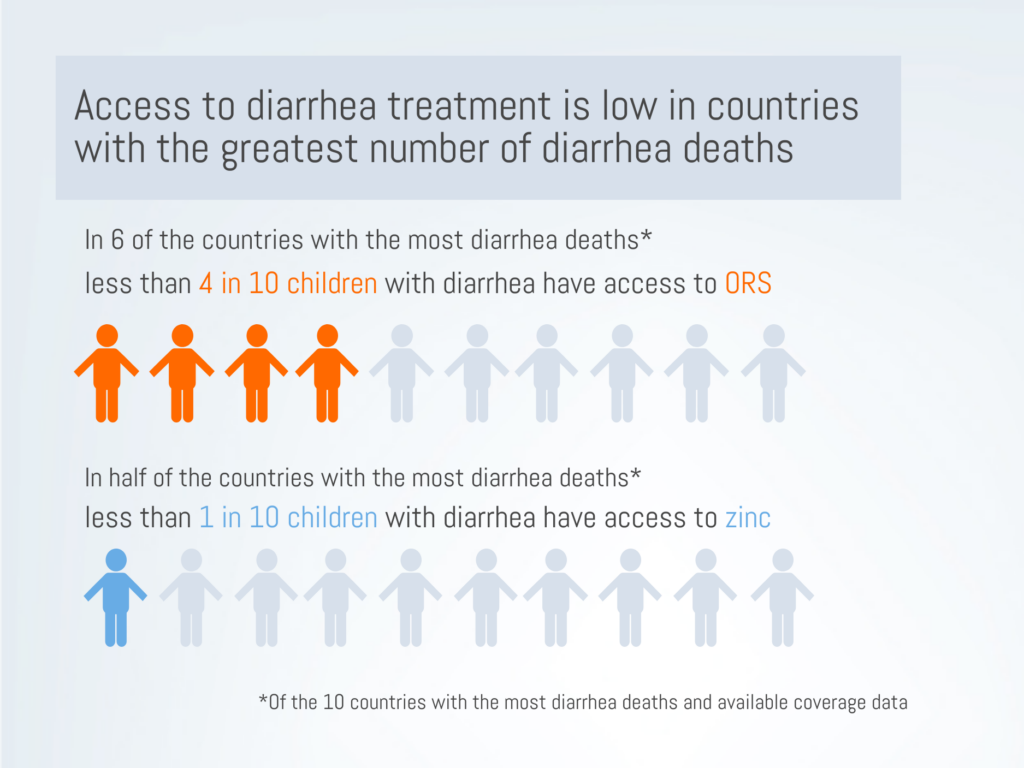
We have highly effective tools to fight diarrhea. Interventions to improve water, sanitation, and hygiene (WASH) have been successful in reducing the number of diarrhea cases.[7] Exclusive breastfeeding for the first 6 months of life can protect infants from undernutrition and its associated vulnerability to diarrhea.[7] Inexpensive but effective treatments like oral rehydration salts (ORS) and zinc supplements work to stop diarrhea episodes from becoming severe and deadly. Yet, access to ORS and zinc is dismally low in many high-burden settings. In 6 of the 10 countries with the highest number of diarrhea deaths[7], national ORS coverage is below 40%.[8] In half of the 10 highest-burden countries[7], fewer than one in ten children have access to zinc supplements. In addition, we also see inequities in access to treatment. In at least half of the 10 highest-burden countries, ORS coverage was at least 10 percentage points lower in rural areas compared to urban areas, or in the poorest 20% of the population compared to the wealthiest 20%.[8]
Vaccination is our strongest protection against vaccine-preventable causes of diarrhea
Two types of common diarrhea are vaccine preventable: rotavirus and cholera. Rotavirus vaccines are especially crucial in preventing a large proportion of diarrhea deaths and hospitalizations around the world. Cholera vaccination is critical in preventing outbreaks in high-risk settings.
Rotavirus vaccination can prevent hospitalizations and death
Although WASH interventions have successfully reduced the global burden of diarrhea, one main cause of diarrhea mortality – rotavirus – is not prevented through WASH interventions.[9],[10] Rotavirus is associated with approximately one third of diarrhea deaths and can only be adequately prevented through vaccination.[2],[9]
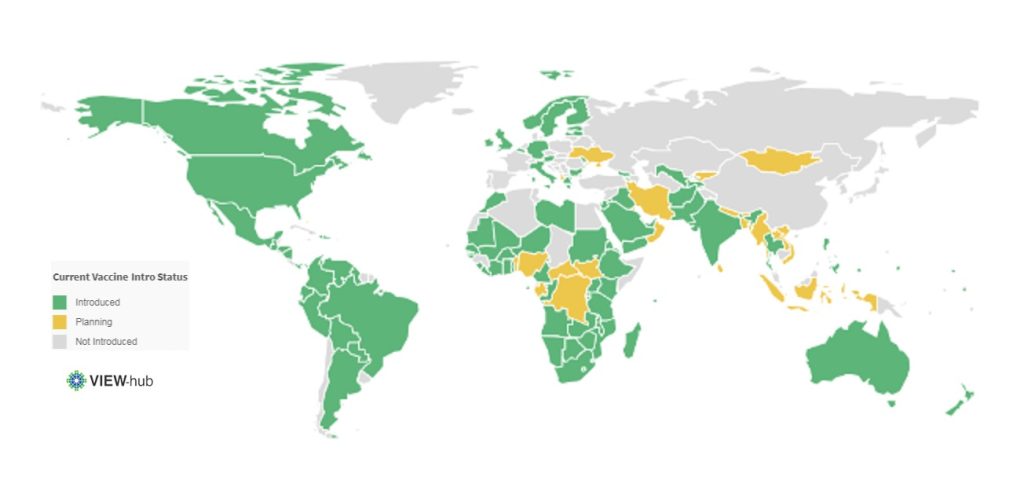
Rotavirus is a leading cause of diarrhea in infants.[5] This highly contagious virus kills about 200,000 children under 5 each year and is responsible for almost 40% of all diarrhea hospitalizations each year.[2],[5] Although ORS can treat simple cases of rotavirus, many of the world’s poorest children don’t have access to ORS.[8] Rotavirus vaccines have proven highly effective and impactful in countries where they have been introduced. In Malawi, for example, there was a 35% decrease in all-cause diarrhea deaths following rotavirus vaccination.[11] Rotavirus hospitalizations in children under 1 year fell by 80% after vaccine introduction.[12] As of January 2019, 97 countries have introduced rotavirus vaccines into their national schedule.[13]
Current Rotavirus Vaccine Introduction Status*
Rotavirus vaccination can protect health systems and resources
Although diarrhea treatment is relatively inexpensive, when we factor in the sheer burden of diarrhea, these treatments are costly to health systems and require substantial health worker capacity. Although many cases of diarrhea can be treated in outpatient facilities with low-cost treatment, inpatient treatment of diarrhea can cost hospitals 25 times the cost of outpatient treatment, per patient.[14]
Treating diarrhea uses limited health systems resources, such as hospital beds, and consequently consumes the resources that can be used to treat other diseases – often diseases aren’t preventable. Therefore, direct and indirect benefits of rotavirus vaccination programs play a critical role in reducing the strain on health systems. One in four children who were taken to a large pediatric hospital in Bangladesh were refused admission to the hospital because all of the beds were occupied. Acute diarrhea was one of the most common reasons for being admitted to the hospital, showing children with acute diarrhea filled many of the available hospital beds. Over half of the acute diarrhea cases that were admitted were due to rotavirus, showing that vaccination could prevent children from both needing and utilizing essential hospital resources.
We’ve seen tremendous reductions in hospitalizations for rotavirus diarrhea and all-cause diarrhea following rotavirus vaccine introductions.[15] A review of rotavirus vaccine introductions found that, globally, all-cause diarrhea hospitalizations reduced by almost 40% in children under 5 in regions where the vaccine had been introduced. The continued use and scale up of rotavirus vaccines will alleviate pressure from over-burdened facilities, enabling health systems to be more responsive.
Rotavirus vaccination may protect families from being pushed into poverty due to treatment costs
Rotavirus vaccination programs can protect the most vulnerable families from medical impoverishment and catastrophic healthcare costs. When looking at all-cause diarrhea In Malawi, the costs associated with treating diarrhea pushed families into poverty, with treatment costs exceeding the monthly income for one in six families needing inpatient care and one in ten families needing outpatient care. Families can be pushed into poverty by the costs of hospitalizing a child with rotavirus for several days. In Malaysia, the inpatient costs of rotavirus treatment can cost families 25% of an average family’s monthly income. Direct and indirect treatment costs, such as medicine and transportation, caused almost 9 in 10 Malaysian families to spend more than 10% of their monthly household income on treating rotavirus.
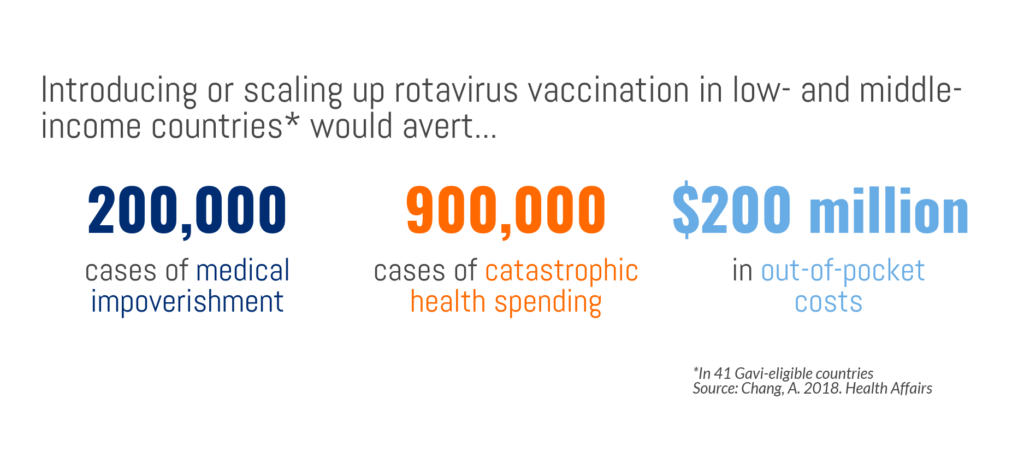
Rotavirus vaccine introduction in 41 GAVI-eligible countries could avert 40% of catastrophic health costs – 900,000 cases – and 40% of medical impoverishment – 200,000 cases. In other words, with rotavirus vaccination programs, 900,000 families would not incur health costs that are higher than a substantial proportion of their income and 200,000 families not would fall below the poverty line due to treatment costs. If rotavirus vaccination programs were introduced or scaled up in Gavi-supported countries, $200 million in out-of-pocket health expenses attributable to severe rotavirus infections could be averted, meaning low-income families would have more disposable income and greater financial stability. With vaccines being one of the more equitable health interventions accessible to poor families, they are an important strategy to reduce the gap in health outcomes by household income as well as protect many families from being pushed into poverty. Inequitable access to treatment, not an uncommon event, only exacerbates the disproportionate risk of mortality in vulnerable children, again underscoring the importance of preventing diarrhea in the first place and protecting children from the vicious aftermath of diarrhea.
Rotavirus vaccination can protect communities
Rotavirus vaccines provide immunity for not only children directly vaccinated but also affords protection to their families and communities. This herd immunity magnifies the public health benefit of rotavirus vaccination by extending protection to those age groups in the population who are not directly receiving the vaccine but can contract and transmit the disease. This additional benefit is essential for a resilient pathogen like rotavirus, that can live on surfaces – and therefore transmit disease – for days. As a result of rotavirus immunized children in the community, rotavirus hospital admissions in unvaccinated children aged two to five years of age, who were not age-eligible to receive the vaccine at the time, were reduced by 41% to 92% in hospitals across the US, showing the profound value of herd immunity.

Cholera vaccination can protect vulnerable groups
Cholera burden
Diarrhea caused by cholera can be rapidly fatal, with as many as 1 in every 5 cases of cholera advances to severe disease.[16] Cholera, often called a disease of poverty, can be endemic and epidemic in settings without strong water and sanitation systems, such as humanitarian emergency settings. Because settings where cholera is most rampant are often those with weak or overburdened health systems, diagnosing and recording cases is difficult; the global estimates of cholera cases each year – between 1.3 and 4 million cases – likely underestimate the true burden.[16]
Unlike many vaccine-preventable diseases, the global number of cholera cases has been steadily climbing for the past 10 years. Devastating cholera epidemics have impacted Yemen, Haiti, Somalia, the Democratic Republic of Congo, and South Sudan in recent years, and continue to be a threat in fragile settings.[17] In addition to the health impacts of cholera, previous outbreaks have led to significant economic losses to countries, caused by reduced revenue on trade and tourism, and continue to threaten countries.[16]
Cholera vaccination
Cholera vaccination is a crucial, cost-effective tool to fight cholera, especially in fragile settings that lack sufficient water and sanitation. In 2013, global partners collaborated to form a stockpile of the oral cholera vaccine, managed by the Global Task Force on Cholera Control and funded by Gavi, the Vaccine Alliance.[16] The stockpile has been utilized for mass vaccination campaigns for prevention in humanitarian crises and for reactive response to outbreaks.[17]
An important – and beneficial – feature of cholera is that vaccinating a relatively small number of people can result in significant herd protection. Research from Bangladesh suggests that 70% vaccine coverage can stop cholera transmission, which greatly amplifies the impact of vaccine campaigns and investments.[18] Cholera vaccination is also a critical tool in managing outbreaks and protecting national and global health security.
Continuing – and strengthening – the fight against diarrheal diseases
Certain types of serious diarrhea can be both preventable and treatable, and a large proportion of child diarrhea deaths can be prevented through vaccination. We have the tools to defeat diarrhea, but these tools are only effective when backed by strong political and financial commitment. The global fight against childhood diarrhea has undoubtedly had a profound impact on child health and broader societal development. Yet, consistently low treatment coverage and constraints in vaccine supply highlight ongoing challenges. These challenges must be responded to with the resources and commitment necessary to pick up the pace of progress, so we can be stronger in the global fight against one of the most common causes of childhood illness and death.
[1] WHO and Maternal and Child Epidemiology Estimation Group, Estimates of child cause of death, diarrhoea 2018. Retrieved from: https://data.unicef.org/topic/child-health/diarrhoeal-disease/
[2] Institute for Health Metrics and Evaluation (2018). Global burden of disease, GBD Results tool. Retrieved from: http://ghdx.healthdata.org/gbd-results-tool
[3] World Health Organization (2017). Diarrheal Disease. Retrieved from: http://www.who.int/en/news-room/fact-sheets/detail/diarrhoeal-disease
[4] Troeger, C., Colombara, D. V., Rao, P. C., Khalil, I. A., Brown, A., Brewer, T. G., … & Petri, W. A. (2018). Global disability-adjusted life-year estimates of long-term health burden and undernutrition attributable to diarrhoeal diseases in children younger than 5 years. The Lancet Global Health, 6(3), e255-e269.
[5] Tate, J. E., Burton, A. H., Boschi-Pinto, C., Parashar, U. D., World Health Organization–Coordinated Global Rotavirus Surveillance Network, Agocs, M., … & Ranjan Wijesinghe, P. (2016). Global, regional, and national estimates of rotavirus mortality in children< 5 years of age, 2000–2013. Clinical Infectious Diseases, 62(suppl_2), S96-S105.
[6] Ibrahim, M. K., Zambruni, M., Melby, C. L., & Melby, P. C. (2017). Impact of childhood malnutrition on host defense and infection. Clinical microbiology reviews, 30(4), 919-971.
[7] WHO/UNICEF (2013). Ending preventable child deaths from pneumonia and diarrhoea by 2025: The integrated Global Action Plan for Pneumonia and Diarrhoea (GAPPD). Retreieved from: https://www.who.int/maternal_child_adolescent/documents/global_action_plan_pneumonia_diarrhoea/en/
[8] International Vaccine Access Center (IVAC), Johns Hopkins Bloomberg School of Public Health. (2018). Pneumonia and Diarrhea Progress Report 2018.
[9] Lamberti, L. M., Ashraf, S., Walker, C. L. F., & Black, R. E. (2016). A systematic review of the effect of rotavirus vaccination on diarrhea outcomes among children younger than 5 years. The Pediatric infectious disease journal, 35(9), 992-998.
[10] Glass, R. I., Parashar, U., Patel, M., Gentsch, J., & Jiang, B. (2014). Rotavirus vaccines: successes and challenges. Journal of infection, 68, S9-S18.
[11] Bar-Zeev, N., King, C., Phiri, T., Beard, J., Mvula, H., Crampin, A. C., … & Costello, A. (2018). Impact of monovalent rotavirus vaccine on diarrhoea-associated post-neonatal infant mortality in rural communities in Malawi: a population-based birth cohort study. The Lancet Global Health, 6(9), e1036-e1044.
[12] Burnett, E., Jonesteller, C. L., Tate, J. E., et al. 2017. Global impact of rotavirus vaccination on childhood hospitalizations and mortality from diarrhea.. The Journal of Infectious Diseases. 215(11), 1666-1672..
[13] International Vaccine Access Center (2018). VIEW-hub: Vaccine Introduction and Epidemiology Window. Retreived from: http://view-hub.org. Accessed January 31, 2018.
[14] Sarker, A. R., Sultana, M., Mahumud, R. A., Ali, N., Huda, T. M., Haider, S., … & Morton, A. (2018). Economic costs of hospitalized diarrheal disease in Bangladesh: a societal perspective. Global health research and policy, 3(1), 1.
[15] Groome, M. J., Zell, E. R., Solomon, F., Nzenze, S., Parashar, U. D., Izu, A., & Madhi, S. A. (2016). Temporal association of rotavirus vaccine introduction and reduction in all-cause childhood diarrheal hospitalizations in South Africa. Clinical Infectious Diseases, 62(suppl_2), S188-S195.
[16] World Health Organization. (2017). Cholera vaccines: WHO position paper–August 2017. Weekly Epidemiological Record. 92(34), 477-498.
[17] Wierzba, T. F. (2018). Oral cholera vaccines and their impact on the global burden of disease. Human vaccines & immunotherapeutics, 1-8.
[18] Dimitrov, D. T., Troeger, C., Halloran, M. E., Longini, I. M., & Chao, D. L. (2014). Comparative effectiveness of different strategies of oral cholera vaccination in Bangladesh: a modeling study. PLoS neglected tropical diseases, 8(12), e3343.
