Last month at the G7 meeting in Canada, global leaders met to consider gender equality, one of the 5 key themes Canada will advance during their tenure. Partners, experts and representatives in the immunization world echoed this emphasis on gender at the Global Immunization Meeting in Kigali, Rwanda just a few days ago. The issues of gender and gender equity within immunization are complex, and designing research to study equity gaps can be difficult. To understand what we do know about immunization and gender, women’s empowerment and gender equity, the VoICE team this month features an overview of these issues.
A selection of VoICE evidence in this issue
Key Points
- Global and national level estimates of vaccine coverage obscure persistent gender inequity in some populations.
- At the national level, gender inequality for women is correlated with higher child mortality and lower childhood immunization rates.
- Reaching higher levels of education greatly increases the likelihood that a woman’s children will be vaccinated.
- The more empowered women are – i.e. have control over family decision-making, financial resources, etc. – the more likely their children are to be vaccinated.
- An equity approach to immunization and child health is both a moral imperative and an efficient use of resources.
Equity matters for the health of women and children
While much progress has been made to reduce child mortality and increase vaccine coverage in the last few decades, inequities still exist from a variety of perspectives, and gender influences vaccine access in several ways. When considering both between and within country inequities; geographic, wealth, and educational for example, female specific gender inequity remains a common thread.
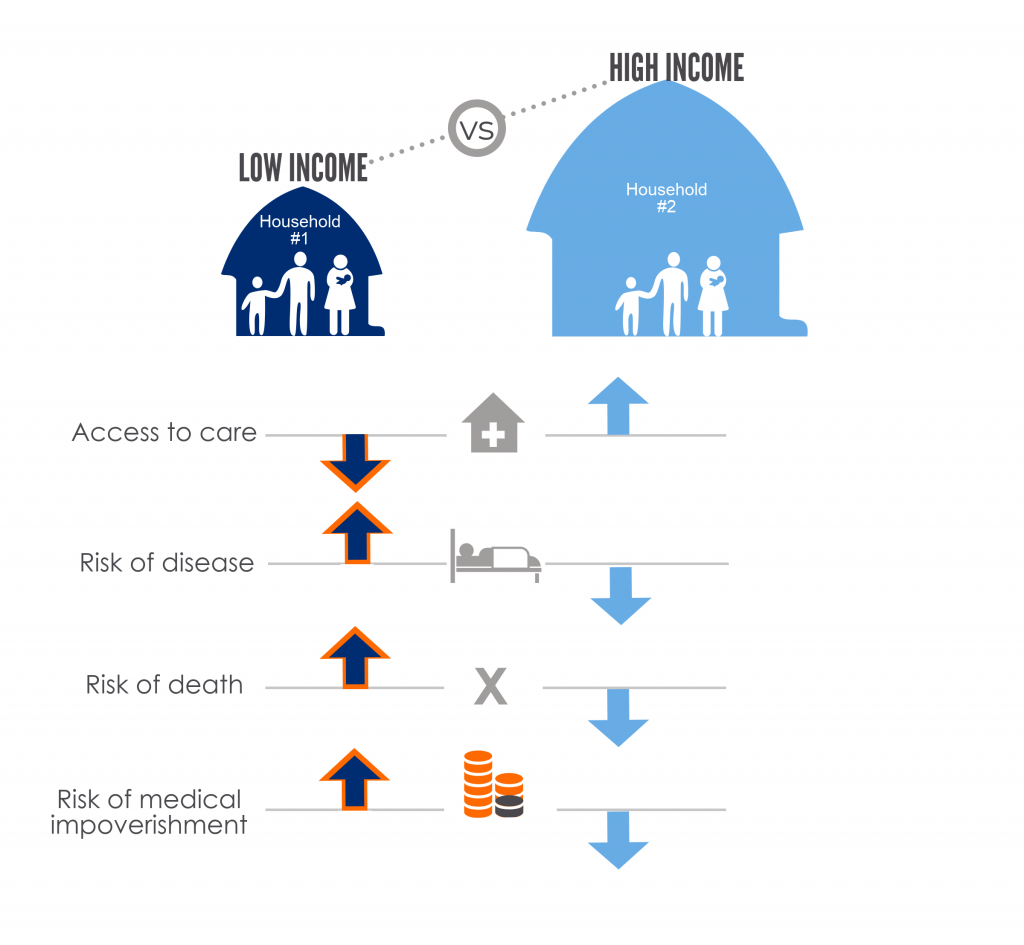
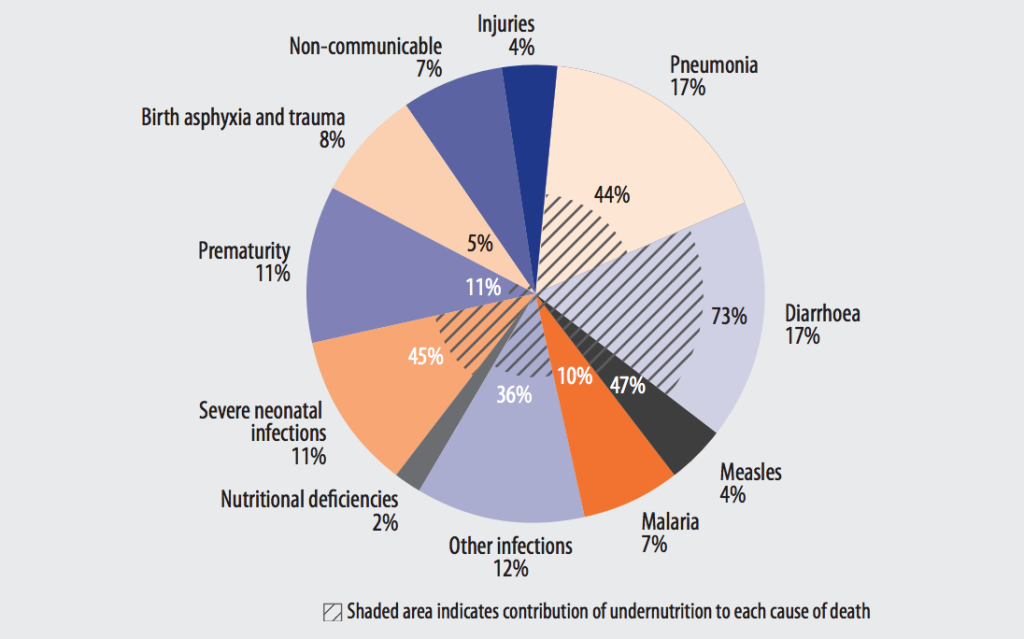
According to UNICEF, children in sub-Saharan Africa are 10 times more likely to die before their fifth birthday than children in high-income countries, a gap that has not changed much in the last 25 years. At the same time, low- and middle-income countries have significantly greater gender inequality and higher under-5 mortality rates than high-income countries. This gender inequality is significantly correlated with lower immunization coverage, and with higher neonatal, infant and under-5 mortality.
Child gender and immunization
In some parts of the world, gender influences a child’s access to vaccines and health care.
Differential vaccine coverage of childhood immunization between boys and girls is an inequity largely invisible at the global level but which persists in certain geographic and social settings. This is reported in studies from regions of the world where there is strong cultural preference for sons over daughters. A study conducted in the urban poor in India which examined household and neighborhood-level determinants of childhood immunization, researchers found that girls were 22% less likely than boys to be fully immunized. This trend has not changed despite increasing overall vaccine coverage rates nationally.
Another study that examined the gender gap in immunization coverage in a rural sub-district of Bangladesh showed that although poverty, low maternal education, and larger number of children in a family decreased the likelihood that any child would be vaccinated, the effect of these factors was more pronounced for girls than for boys. In other words, given the same set of pressures on families that negatively impact immunization, girls fared worse than boys in terms of likelihood of receiving vaccines.
There is a small amount of evidence that girls have less access to care if sick in specific settings. In an Indian study from the northern state of Bihar, girls who were ill were less likely to receive care in a health facility than boys, although the study did not find different rates of immunization coverage between the sexes.
Gender differences in child health care utilization for both prevention and treatment of disease may be a contributing factor driving excess mortality for girls in South Asia. South Asia is the only region of the world in which a slight natural survival advantage in female infants compared to male infants is reversed. This means that in South Asia, male infants have a better chance of surviving to their first birthday than females. It is estimated that the excess female infant mortality in India results in 9 additional deaths/1000 live births of girls compared to boys, and this disparity has worsened since 1990.1
Critically, it must be acknowledged that local attitudes and motives that underpin vaccination and health seeking behaviors can vary significantly between countries and communities and are often driven by a set of complex interrelated factors that, in addition to gender, include parental education, socioeconomic status, geographic access, cultural preferences and biases.
Mothers and childhood immunization

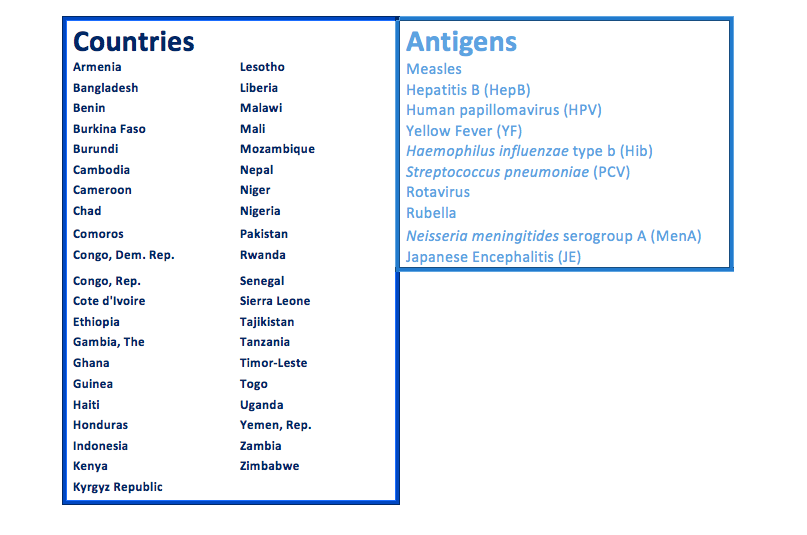
Gender equality for women, and maternal empowerment in particular, are factors which can significantly influence the health of children and a child’s access to immunization. Two recent studies have examined this relationship between child health and overall gender equity at the national level. In a 2015 study looking at the degree of gender inequality among 138 countries with data from the United Nations Development Program, greater inequality between women and men was significantly correlated with a country having higher under-5 mortality rates and lower immunization rates. A second study found that among 45 low- and lower-middle income countries supported by Gavi, countries with the least gender equality (as measured by reproductive health, women-held parliamentary seats, educational attainment and other factors) also had lower vaccine coverage rates overall.
There are many ways in which a woman’s empowerment affects the health of her children. A child’s health – including the likelihood that they will be immunizated – in turn benefits from programs and policies that empower and educate women.
Educating women means children are more likely to get vaccinated
Studies have shown that maternal education is significantly associated with children’s immunization coverage. Researchers looking at vaccination coverage in 45 low- and middle-income countries found that children of the least educated mothers are 55% less likely to have received measles-containing vaccine and three doses of DTP vaccine compared to children of the most educated mothers. Another study looking at WHO data from member states shows that globally, coverage of the third dose of DTP is 26% higher among children born to mothers with some secondary education compared to mothers with no education. The increased likelihood of timely vaccination likely plays a role in the improved chances of child survival that are also associated with maternal education. An analysis conducted by UNICEF in 2015 found that across many South Asian and sub-Saharan African countries, children with mothers who received no formal education were almost 3 times more likely to die before reaching age 5 than those born to mothers with some secondary education.
The influence of empowerment and agency
Education is one important component or ‘resource’ that can empower women, but another key factor is a woman’s agency – her ability to define, and take action towards, personal goals. The degree of agency a woman may have is mediated by factors such as power over decision-making, access to money, social status, and freedom of movement. A 2016 systematic review of studies covering forty years of data from primarily African and Southeast Asian countries, found a trend where higher levels of women’s agency were linked to higher likelihood of complete immunization for their children. In another systematic review, in which qualitative research from low- and middle-income countries was analyzed to understand gender-related reasons for low vaccination rates, women’s low social status was shown to be a barrier to accessing vaccinations for their children. Specifically, key drivers of likelihood of vaccination included maternal education, family income, as well as a woman’s ability to control resource allocation and autonomous decision-making related to how her time is used.
One explanation for this effect may be that as agency increases, a woman may have more decision-making power to choose how household resources such as money and time are allocated; and if given the means, women often prioritize children’s health. In effect, her children’s good health is the goal towards which she will apply available family resources, to the degree her level of agency and resources allow.
Enticing evidence from one study indicates that empowerment and its positive benefits can be contagious. In a study of the impact on child immunization rates of a women’s empowerment program conducted among socially and economically disadvantaged women in India, it was noted that not only were the children of the women who had direct participation in the program immunized, but there was a measurable spill-over effect of vaccination to non-participants in program villages. Non-participating children in villages where the program occurred were anywhere from 9 to 32% more likely to be immunized against measles than children in villages without the empowerment program.
What can progress toward gender equity look like?
Sustainable Development Goal (SDG) 5
The Sustainable Development Goal (SDG) 5—to achieve gender equality and empower all women and girls—is a goal that is inextricably linked with progress on many fronts, particularly in the arena of women and children’s health. Similarly, the achievement of SDG 3 – to ensure healthy lives and promote wellbeing for all at all ages – rests on many factors, but both immunization and a concerted focus on gender disparities in low-income countries will be absolutely essential to this goal.
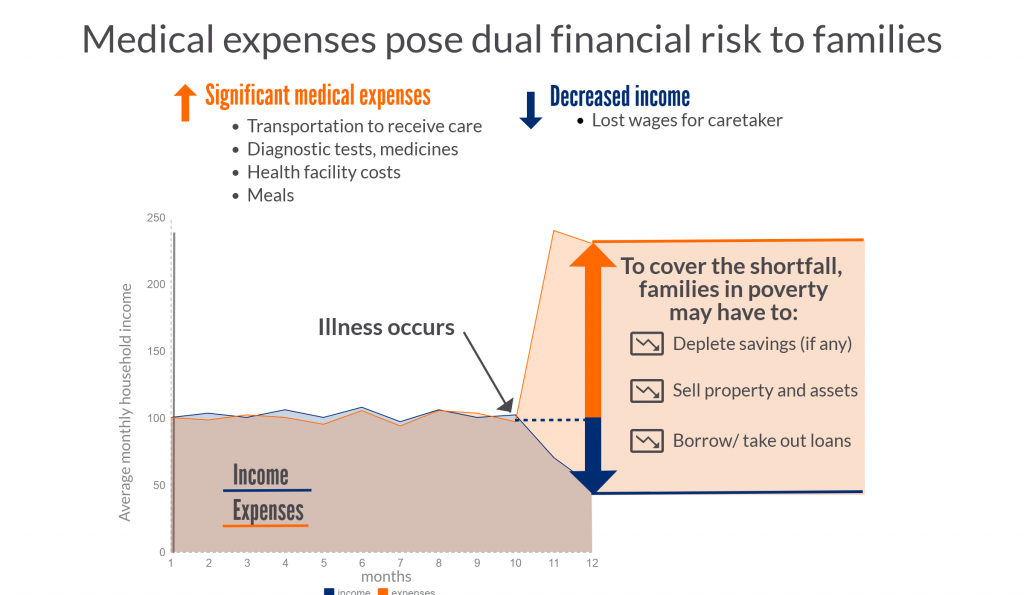
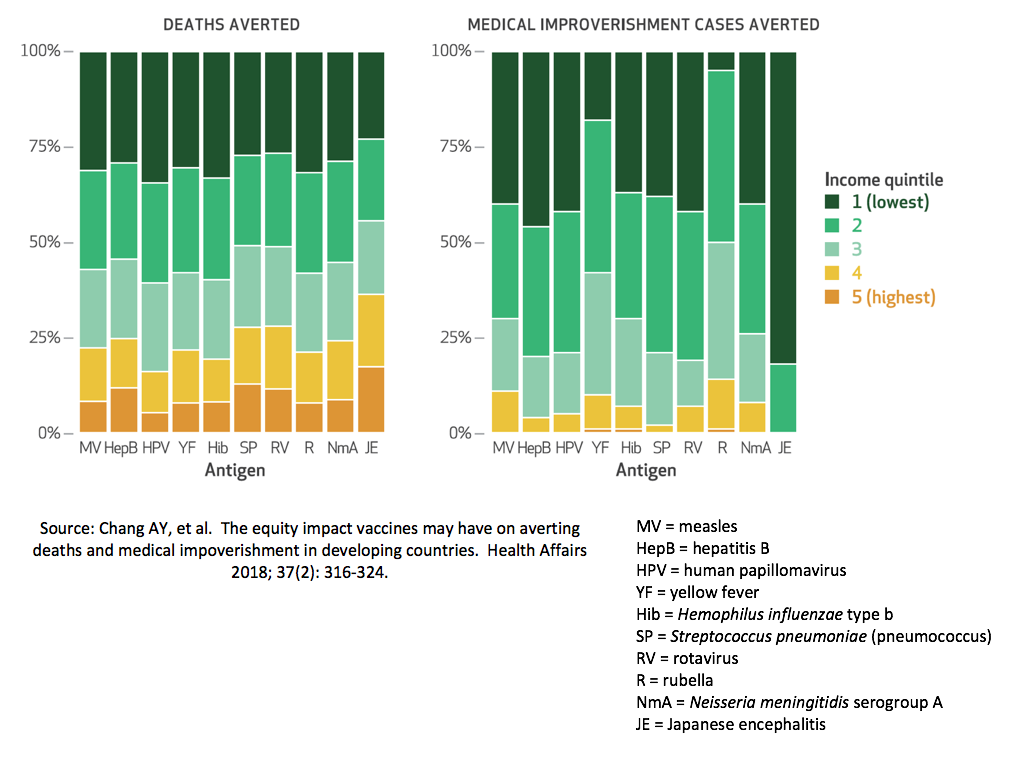
This focused approach on inequity makes both practical and financial sense. A 2010 study from UNICEF concluded that an equity-focused strategy would hasten progress towards health goals and be cost-effective, especially in low-income, high-mortality countries.2 Specifically, investment in a package of interventions designed to increase health equity, including access to immunization, was estimated to improve child mortality reductions by more than 20% over the status quo. Focusing programmatic efforts and supportive policies on the poorest or worst off in a population yields the greatest positive change with limited resources. Equity analyses can aid decision-makers in understanding both who is left behind or left out of progress on health and social fronts, and why.
Strategies which specifically target the health of women and children in an integrated way across interventions may be able to reverse gender inequity in immunization in some contexts. The National Rural Health Mission in Haryana, India, for example, implemented a multi-strategy community intervention program intended to reduce maternal and child health inequalities by improving healthcare at the household level in villages. Through the use of local incentives including cash, payment of travel costs, free hospital services for pregnant women, hospital-based treatment of neonatal illnesses, and locally appointed Health Activists, the program was able to eliminate gender inequalities for full immunization between male and female children. While such synergy between immunization visits and essential health care can be more involved to implement programmatically, the collateral gains make it worth pursuing in the service of creating healthier, more equitable societies.
Although much work has been done to identify child and family dynamics that underpin gender inequalities, more research and attention is needed to create change at the local and regional levels. Tailored strategies will be necessary in each setting to improve women’s agency and eliminate differential vaccination coverage for girls. Concentrating resources to improve gender equity in access to health will be integral to attaining global immunization and child survival goals, and can reinforce efforts to empower women worldwide.
For Additional Information:
1Alkema L, Chao F, et al. National, regional, and global sex ratios of infant, child, and under-5 mortality and identification of countries with outlying ratios: a systematic assessment. Lancet Global Health 2014; 2: e521-530.
2UNICEF. Narrowing the gaps to meet the goals, UNICEF, New York, September 2010.